Scientists pinpoint protein that helps cancer-causing viruses evade immune response
The viruses Kaposi sarcoma-associated herpesvirus (KSHV) and Epstein-Barr virus (EBV) have been linked to several cancers. For the first time, UNC School of Medicine scientists have discovered that these viruses use a human protein called barrier-to-autointegration factor 1, or BAF, to evade our innate immune response, allowing the viruses to spread and cause disease.
These findings, published in Nature Communications, suggest that BAF and related proteins could be therapeutic targets to prevent these viruses from spreading and leading to cancers, such as Kaposi sarcoma, non-Hodgkin lymphoma, Hodgkin lymphoma, multicentric Castleman disease, nasopharyngeal carcinoma, and gastric cancer.
“Viruses are in a constant battle with the cellular immune system, which includes the protein cyclic GMP-AMP synthase, or cGAS, which binds to viral DNA and sounds the alarm to trigger immune responses and fight the viral invaders,” said senior author Blossom Damania, Ph.D., the Boshamer Distinguished Professor of Microbiology and Immunology and member of the Lineberger Comprehensive Cancer Center. “We’ve discovered that KSHV and EBV use a different host cell protein, BAF, to prevent cGAS from sounding the alarm.”
Viruses have evolved with humans for millions of years, so it’s no surprise they’ve evolved tricks to evade our natural, or innate, immune responses. Finding out precisely how viruses do this is the basis for creating vaccines and therapeutics to overcome their tricks.
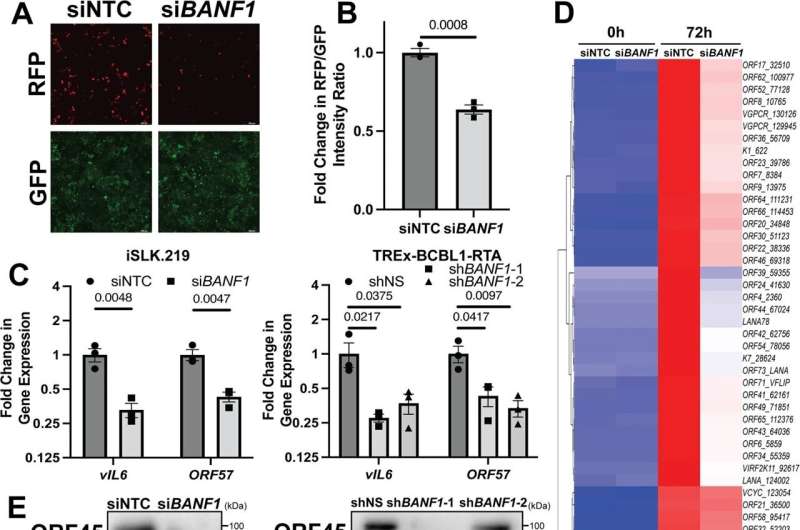
In the case of KSHV and EBV, the expression of BAF is increased upon infection, suggesting that these viruses take advantage of this host protein to blunt the immune response to infection. In a series of experiments, Damania’s lab found that BAF contributes to the degradation of the cGAS DNA sensor. With less cGAS protein available in the infected cell to detect DNA, the cells mount weaker immune responses, which allows these two viruses to replicate and spread more efficiently.
“BAF enables EBV and KSHV to reactivate from latency, replicate, and make more of themselves,” said first author Grant Broussard, a graduate student in the Genetics and Molecular Biology Curriculum at UNC Lineberger. “Our study highlights the prominent role that DNA detection pathways like the cGAS pathway play in controlling viral infection.”
He stressed that disrupting BAF activity with targeted therapies could reduce its immunosuppressive effects, thus restricting replication of these viruses to prevent the spread of disease.
Damania, who is a Leukemia and Lymphoma Society Scholar and a Burroughs Wellcome Fund Investigator in Infectious Diseases, added, “Preventing lytic replication will prevent transmission of these viruses and also reduce the global cancer burden associated with these two viruses.”
More information:
Grant Broussard et al, Barrier-to-autointegration factor 1 promotes gammaherpesvirus reactivation from latency, Nature Communications (2023). DOI: 10.1038/s41467-023-35898-2
Journal information:
Nature Communications
Source: Read Full Article