Subset of Patients With Melanoma Have Very Low Mortality Risk
Although melanoma is the most serious skin cancer, most patients do have high chances of survival. New research has now identified a subset of patients with early disease who have a very low risk of dying from the disease.
In a cohort of almost 11,600 patients, the overall 7-year rate of death from melanoma was 2.5%, but the risk in a subset of 25% of patients was below 1%.
Conversely, the study authors were also able to identify a small subset of high‐risk patients with a greater than 20% risk for death.
Though more data are needed and the findings verified in other studies, the use of a different term such as “melanocytic neoplasm of low malignant potential” may be more appropriate and may help to begin to address the problem of overdiagnosis, they note.
“While the topic of very low risk melanomas has been presented at national and international meetings, there have been no formal discussions to define the classification of ‘melanocytic neoplasms of low malignant potential’ at this time,” first author Megan M. Eguchi, MPH, of the Department of Medicine, University of California, Los Angeles, said in an interview. “Criteria would need to be established using study designs beyond those available using SEER data.”
She emphasized that currently, they do not propose any change to treatment of these lesions, just a change to the terminology. “A diagnosis of ‘MNLMP’ rather than ‘melanoma’ may potentially alleviate people’s concerns related to prognosis and begin to address the problem of overdiagnosis,” said Eguchi.
The study was recently published online in Cancer.
Even though melanoma is considered to be the most common potentially lethal tumor of the skin, prognosis is often very good for those with T1 tumors, the lowest risk category. Prognostic modeling has been used to predict survival in patients with melanoma and identify prognostic variables, the authors note, with the most prominent attributes being Breslow thickness and ulceration of the primary tumor, which form the basis of the current American Joint Committee on Cancer (AJCC) staging system.
There is evidence that the increasing incidence of melanoma is partly due to overdiagnosis, meaning the diagnosis of lesions that will not lead to symptoms or death. The authors write that they were interested in identifying lesions that are currently diagnosed as melanoma but might lack the capacity for metastasis, cases that could potentially be part of the phenomenon of overdiagnosis.
Subsets With Low and High Risk for Death
In the study, Eguchi and colleagues analyzed information from the US Surveillance, Epidemiology, and End Results (SEER) database and identified 11,594 patients who were diagnosed in 2010 and 2011 with stage 1 melanoma that was ≤ 1.0 mm in thickness and had not spread to the lymph nodes. Prognostic models for risk for death from melanoma in patients with low-risk melanomas were developed, and then the ability of the models to identify very‐low risk subsets of patients with melanoma‐specific survival surpassing that of T1 overall was evaluated.
The median age of the patients was 58 years, the median Breslow thickness was 0.45 mm (interquartile range [IQR], 0.30-0.65 mm), and 71% were assigned stage IA. Ulceration was present in 4% of cases, 27% were mitogenic, and 45% were Clark level II, and within this cohort, 292 (2.5%) patients died of melanoma within 7 years. In the training data set, 177 of 7652 (2.3%) patients died of melanoma within 7 years, and numbers were similar in the testing set (115 of 3,942; 2.9%).
Overall, the investigators identified three large subsets of patients who were in the AJCC seventh edition classification for stage I (“thin”) melanoma, who had a risk for death of approximately less than 1%. This was a marked improvement from the rate of the overall sample. In the simplest model (Model 1A), patients who were younger than 70 years at diagnosis with Clark level II invasion were deemed as very low risk.
In Model 1B, the same initial classification was used, but it was further refined and limited to patients who were either age 43 years or younger or 44-69 years with Breslow thickness < 0.40 mm. At 10 years postdiagnosis, this subset also showed a less than 1% risk for death from melanoma. The logistic regression model (Model 2) was similar, as it identified about 25% of patients with a predicted risk for death of less than 0.5%, incorporating patient age, sex, mitogenicity, Clark level, and ulceration. Model 2 was also able to further identify a small subset of patients with no deaths.
The logistic regression model was also able to identify a very small subset (0.7% and 0.8%) of patients who had a risk for death that exceeded 20%, which was markedly higher compared with most patients with T1b tumors.
More Data Needed
Commenting on the study, Beth Goldstein MD, a dermatologist and co-founder of Modern Ritual Health, Chapel Hill, North Carolina, noted that in the future, when there is the ability to determine which lesions have an aggressive biologic potential, “then ideally, we can avoid unnecessary removals.”
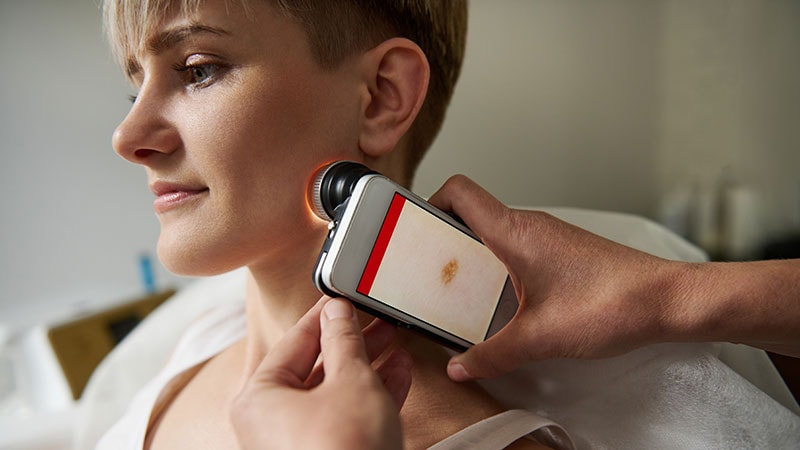
“At this point, there is the option of genomic testing to screen in vivo for melanoma,” Goldstein told Medscape Medical News. “While this can reduce unnecessary procedures, the costs to the healthcare system are significantly higher at this time compared to a limited removal. Confocal microscopy can reduce procedures but again is not widely available, adds costs to the healthcare system, and cannot determine the aggressive nature of a melanocytic lesion in vivo.”
Goldstein acknowledged that there are unnecessary procedures done perhaps for lesions that would never become life threatening, but at the same time, it is known that there are certain early lesions that are more likely to metastasize and are only known after a complete removal and pathologic assessment.
In addition, besides concerns with removing a suspicious lesion, such as scarring, “there is very limited morbidity associated with this procedure,” she said. “At this time, most patients with early melanomas do not require more than an outpatient procedure under local anesthetic and are already reassured of the low-risk nature of their early melanoma.”
Currently, “we do not have the ability to differentiate these tumors further from the initial assessment,” Goldstein continued. “While there is an ability to screen melanomas for higher likelihood for metastasis with the 31 genetic expression profile test, there is still much work to be done to refine these resources.”
This study was supported by National Cancer Institute. Eguchi has no disclosures. Goldstein has no disclosures
Cancer. November 7, 2022. Article
Roxanne Nelson is a registered nurse and an award-winning medical writer who has written for many major news outlets and is a regular contributor to Medscape.
For more news, follow Medscape on Facebook, Twitter, Instagram, and YouTube
Source: Read Full Article