No evidence that ‘overlapping surgery’ to reduce hospital waiting lists will increase number of operations
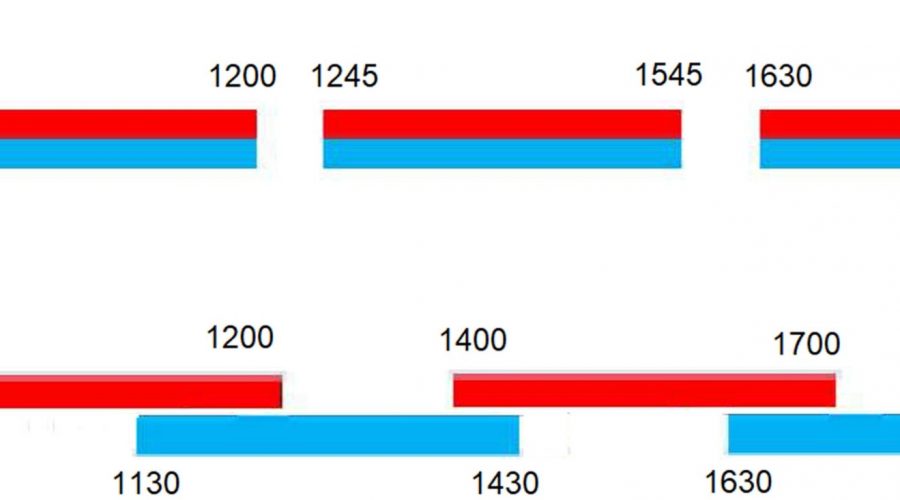
![Data from Padegimas et al. [17] for their examples of (a) two parallel, independent operating lists (Theater 1 (red) and Theater 2 (blue)) each with three cases of 3-h duration and a turnover time between cases of 45 min and (b) an overlapping model where the Theater 1 (red) list resembles that in (a) and the cases in the Theater 2 (blue) list are staggered such that anesthesia commences to enable the senior surgeon from the Theater 1 (red) list to start Theater 2 (blue) surgery after the critical portion in Theater 1 (red) is complete. Note that this overlapping model can, within the time available, only deliver four completed cases vs. six in the conventional model shown in (a). Credit: <i>Anaesthesia</i> (2022). DOI: 10.1111/anae.15797 No evidence that 'overlapping surgery' to reduce hospital waiting lists will increase number of operations](https://scx1.b-cdn.net/csz/news/800a/2022/no-evidence-that-overl.jpg)
Overlapping surgery, in which a single senior surgeon operates across two parallel operating theaters and anesthetists induce anesthesia and junior surgeons commence and complete the operation, has been discussed as a potential route to reducing hospital waiting lists in this post-COVID era in which many patients are expected to face extensive delays of months or even years to have surgery.
However, the authors of a paper published in Anesthesia—led by Professor Jaideep Pandit of Oxford University Hospitals NHS Foundation Trust, U.K.—explain that, while there is potential for overlapping surgery to have some positive impact in situations where turnover times between cases are long, operations are short (two hours or less) and where critical portions of surgery constitute about half of the total operation time, any advantages must be balanced against safety, ethical and training concerns.
Getting a single senior surgeon to move across two operating theaters will maximize the time this senior surgeon spends actually operating, which at first sight seems beneficial—there appears to be less “wasted” turnaround or gap time between cases for this surgeon. Consequently, some NHS Trusts are trialing versions of overlapping surgery as high-intensity theater (HIT) operating lists.
However, the downside of the one senior surgeon eliminating their own wasted time is that all other members of the team—across two operating theaters—increase their own downtime, needing to wait for the surgeon to move across theaters. Moreover, there have been examples of disastrous rollouts of an overlapping surgery policy in the US. One of the world’s leading hospitals, the Massachusetts General Hospital (Boston, MA, U.S.) has paid out more than £26 million (around US$33 million, €31 million) (without liability) to settle cases in relation to its overlapping surgery scheduling policy.
A driver for the lawsuits has been the lack of proper consent: patients (and insurers) did not know the senior surgeon would not be present throughout the surgery. Any financial gains conceived by that policy have been wiped out several times over, and the reputational damage, reduced staff morale and fractured working relationships remain ongoing challenges. The unredacted emails revealed during these court proceedings show how the concerns of many clinicians went unheard by their senior management team.
Prof Pandit and colleagues also cite evidence from Canada showing overlapping surgery led to an almost doubling of risk of complications for both hip fracture and hip arthroplasty, The greater the overlap, the more risk there is of overlap impinging on the “critical portion” of the surgery and therefore, the greater the risk of harm.
Prof Pandit and colleagues also show, for the first time, that the productivity gains cited in support of overlapping surgery are false. It is inevitable that if an extra operating theater is available to a single surgeon, then that surgeon’s number of cases will increase as compared with operating from just one theater. However, it is impossible (for mathematical reasons shown in the paper) for this to exceed the number of the same operations performed by two surgeons in separate theaters. The authors say: “The real question is how productivity of one surgeon working across two overlapping operating theaters compares with two surgeons focused on their own lists.”
That said, overlapping surgery could be useful in the U.K. NHS in hard-pressed specialties where there are not enough surgeons to staff more than one theater; or where only one surgeon has volunteered for extra evening/weekend lists where there are anesthetists and nursing staff available to cover the extra theaters.
Source: Read Full Article