Tough yet flexible treatment for babies in the womb
In children with spina bifida, the neural tube that forms the spinal cord and brain doesn’t close as it should during early prenatal development. That leaves the nerves of the spinal cord exposed to potential damage from fetal movement and from the surrounding amniotic fluid. So while surgeons can repair spina bifida soon after birth, the ideal would be to cover the exposed area during gestation, to protect the developing spinal cord.
What’s been lacking is a surgical adhesive that itself can withstand fetal movement and growth, as well as submersion in amniotic fluid, and is selective in what it sticks to. A new, nontoxic adhesive gel tested at Boston Children’s Hospital could fit the bill. Dario Fauza, M.D., Ph.D., a general surgeon affiliated with Boston Children’s Maternal Fetal Care Center, believes it could improve prenatal surgery for spina bifida and perhaps other defects requiring a patch.
Inspired by the sticky secretions of the dusky arion slug, the gel was developed at the Wyss Institute for Biologically Inspired Engineering and the Harvard School of Engineering and Applied Sciences (SEAS).
“This collaboration was truly a team effort that brought together surgical and bioengineering expertise to address an important unmet clinical need,” said Benjamin Freedman, Ph.D., a Postdoctoral Fellow at the Wyss Institute and SEAS who co-created the technology. “We had previously tested the tough adhesives in many living model systems, but none quite as complex as fetal surgery. We were blown away that the materials performed so well in this challenging setting.”

Putting a slug-inspired gel to the test
Learning of its good performance in sealing heart, skin, and liver tissues, Fauza decided to try it in fetal surgery, starting with spina bifida.
“The fetal environment poses unique challenges for surgical adhesives, particularly in the setting of spina bifida,” said Fauza. “These include continued exposure to the chemically complex amniotic fluid and the fast growth rate of the fetus in the later stages of gestation.”
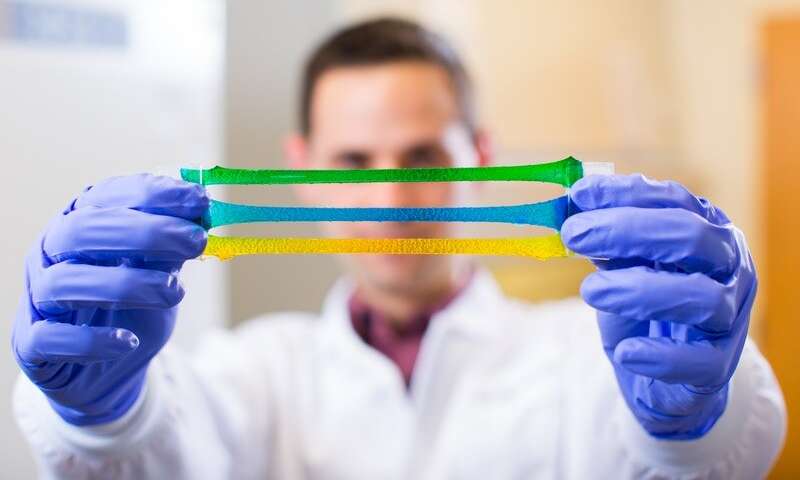
The new gel consists of two components: a hydrogel made of two bound polymer chains (alginate and polyacrylamide), linked to an adhesive polymer (chitosan). Boston Children’s surgical fellows Stefanie Lazow, M.D. and Daniel Labuz, M.D. tested the gel the lab and in a prenatal rabbit model of spina bifida.
As the team reported in the Journal of Pediatric Surgery, the gel proved durable, strong, and flexible. Patches made from it adhered firmly around the edges of the spina bifida defect. As the fetus grew, the gel expanded, and remained in place in 70 percent of the animals tested (and eventually, as the surgeons honed their technique, in 100 percent).
“With some conventional forms of repair, the spinal cord can become tethered to the prosthetic materials, a complication that can negatively impact spinal cord function,” said Fauza. “This new material allows for selective adhesion only to the periphery of the spina bifida defect, but not to the spinal cord. For adhesion to occur, both components must interact with the tissue, which can be controlled by the surgeon.”
The gel stood up to a battery of other tests, including submerging it in amniotic fluid and exposing it to hydraulic pressure mimicking the uterine environment. It kept wounds sealed even when wet, and even on moving surfaces. In the animal model, it survived the rigors of the intra-uterine environment. And it appeared not to interact biochemically with fetal tissue, causing no inflammation or other toxicity. There was even some suggestion that the gel promoted wound healing, rather than simply acting as a patch.
The team’s next steps will be to test the gel in larger animal models with longer gestation times (as opposed to 32-33 days in the rabbit model). They will also explore ways of introducing the gel less invasively, using a scope and a port site into the uterus, rather than open surgery.
Source: Read Full Article
