The Role of Glycans in the Cell and Glycans Imaging Method
 Thought LeadersRichard Drake Professor & Endowed Chair in Proteomics Medical University of South Carolina
Thought LeadersRichard Drake Professor & Endowed Chair in Proteomics Medical University of South CarolinaIn this interview, News-Medical talks to a pioneer of glycan imaging, Richard Drake about glycans, their role in maintaining cellular homeostasis, glycopeptide analysis, and method development for glycan imaging.
What are glycans, and why are they important to biology?
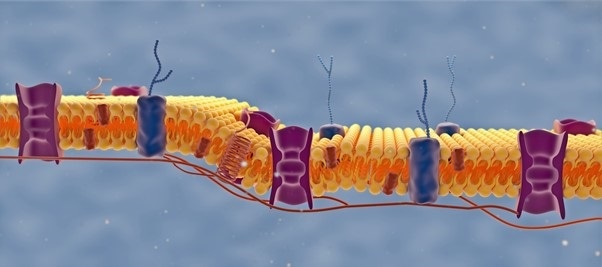
Glycans are complex carbohydrates derived from basic glucose and glutamine metabolism. These glycans are metabolized in complex carbohydrate structures on the cell surface, creating an outer shell on the cell surface termed the ‘glycocalyx.’
Functionally, glycans are involved in protein folding, protein sorting, protein secretion, cell-cell recognition on the surface, organelle and cellular localization, and, more importantly, immune recognition.
What is there to learn from mapping glycan distributions in tissues?
Glycans on the cell surface help to maintain normal cellular homeostasis and health in general. If they get modified, especially in disease scenarios, they tend to get much larger and complex.
These are ideal targets for MALDI imaging, especially if you have the tissues for disease states. This also links well with emerging single-cell methods to look at glycan profiles and clinical imaging and radiology.
Tracking Tumor Progression by Glycan Imaging Mass Spectrometry – Prof. Richard Drake from AZoNetwork on Vimeo.
Does glycan imaging have any clear advantages over other molecular imaging techniques?
There are many practical advantages to glycan imaging; its simple, fast, reproducible and robust signal detection is at its core.
One of the advantages of the assay is that we are spraying an enzyme that creates the signal we detect, so we only detect what the enzyme cleaved. We are also discovering that there are 25 to 30 glycans that are very robustly detected in anything that could be considered alive. This method is very reproducible and very definable.
These glycans can vary in their intensities, and this is where we get into disease differences. This allows us to work with larger clinical cohorts, making our studies reproducible and relatively fast. This opens up a lot of clinical diagnostic opportunities.
The assay works on formalin fixed tissues so that we can get these directly from pathology collections. Millions of these tissues are available, so finding clinically important tissues to run has always been straightforward.
Image Credit: Marco G Faria/Shutterstock.com
Have you found any correlations between individual glycans and cellular diseases? If so, would you describe it as being more diagnostic or prognostic?
We are finding that they are both potentially diagnostic, as well as prognostic. There is increasing evidence that the levels of ‘high mannose structures’, which are biosynthetic precursors to all the other complex glycans, are indicative of the metabolism of a tumor cell or an immune cell, for instance.
We have also seen that in particular tumor subtypes – for example, a mucinous or a neuroendocrine tumor – there are very specific classes of glycan structures. The consistent hallmark of these structures are the presence in the tumor of large tetraantennary N-glycans with multiple fucose sugars. Interestingly, the numbers of fucose residues varies with organ type, as well as other sugar modifications.
What can you say about the correlation between distributions of glycans and originating glycoproteins?
We are finding that there are many correlations between biofluids and tissues, and defining these is the subject of ongoing research.
We found that the method works so well on tissues that we could export it to biofluids, which has expanded into many different technologies. We have a method now where we can profile virtually any biofluid for glycan content.
In addition, we found that we could adapt this method to antibody arrays. This opened up a whole new avenue where we could target serum glycoproteins and glycotype, for example, for each serum glycoprotein. This was never possible in an array-type format.
Now that we have the ability to look at the biofluids, whether via total glycan profiling or with the antibody arrays, we formed GlycoPath as a means and vehicle to develop clinical diagnostics at the biofluid level; but also to link that back to tissues.
As we use tissues that have come straight from pathology, we are increasingly using immunohistochemistry techniques to link the glycans with a particular strain of a glycoprotein or target.
More recently, we have been looking at COVID-infected tissues, and we have been able to link where the spike glycoprotein and immune cell clusters are with different glycans that are present.
We’ve also started looking at classic tumor antigens that are carbohydrate-based in pathology and immunohistochemistry terms. We were able to link these with tumors and the glycans that we detected.
Image Credit: Alpha Tauri 3D Graphics/Shutterstock.com
To researchers studying protein distributions using common tissue imaging strategies like immuno-based imaging, would glycan imaging give increased insight into disease pathways?
Absolutely. At the moment, I cannot think of any scenario where glycan imaging would not complement current immunostaining methods. Signaling regulators, oncogenes, growth factor genes, transcripts or, indeed, anything that is changing the activity of the cell is going to show up in the glycan code on the surface.
This method is particularly useful given the CRISPR-Cas9 revolution taking place with all the genetic models that can be made by knocking in or knocking out individual genes.
If you take any CRISPR-Cas9 animal and knock in or knock out a gene involved in metabolism or growth regulation, a change in glycan will be observed.
Most, if not all, current cancer immunotherapies are targeting surface glycoproteins that regulate immune function. All of these immune checkpoint proteins are glycosylated, and it is already documented that changes in the glycosylation of these targets also affect the treatment outcome.
Going after these immunotherapy-treated tissues is one of our major targets moving forward.
From all the glycan images produced in your lab, what observation would you say has been most exciting?
Asking which observation is my favorite is like asking what my favorite beer is – it is a very time and place dependent answer, and the default response is ‘the beer I haven’t had yet.’ It is the same with glycan imaging. Every time I run a new tissue, there is something new and exciting in the result.
However, there have been some milestones, particularly in 2012 when we did the first image that showed that the method was working, and in 2013, when we ran the first FFPE tissue and showed it could work with archived tissues. These moments opened up the floodgates for a lot of other methods.
Another highlight was the first time we ran a neuroendocrine tissue from the prostate. I could tell immediately that this was very different from everything else we had analyzed so far. It was the first time we had seen the large numbers of tumor associated glycans with multiple fucose residues. We now know this is a hallmark of neuroendocrine tumors from all tissue types.
It has also been great to work with Joe Ippolito, a radiologist at Washington University, who provided the neuroendocrine tumor tissues. This collaboration has morphed into many studies where we are trying to link what we are seeing in these types of prostate tumors with clinical imaging.
Going in the other direction towards single-cell analysis, we are doing some very exciting work with Mike Angelo at Stanford University, linking the glycan imaging with his multiplexed cell and immune targeted probes directly on the same tissues. This is opening up a whole new avenue for multimodal analysis.
Recently, we have just started a collaboration with nephropathologists Jan Braesen and Jessica Schmitz at Hanover Medical University, and they provided some fantastic new tissues in the immunotherapy space. I’m very excited about the initial results and where this is going.
As a pioneer of glycan imaging, what have you found to be the biggest misconception that prevents researchers from starting a glycan imaging study?
I think the biggest misconception about starting glycan imaging starts with one word: glycophobia. Fear of the structural and biological complexity and nomenclature associated with glycans. There are a lot of reasons for this issue – some of these reasons are educational because I don’t think this is specifically taught anymore at most institutions.
Even if you start learning about this field, there are a lot of archaic terms and a whole other language and vocabulary to contend with. It seems complicated because it is not a template-driven synthesis.
To help people with their glycophobia, we conduct different outreach types, including seminars, presentations, as well as provide information on our GlycoPath web page and other websites.
We work with Bruker and the Bruker-MUSC Center of Excellence for Clinical Glycomics to support the development of these methods. We are here to help cure glycophobia, so if anybody wants to learn about the methods that we use, reach out and contact us.
What do you see the future of glycan imaging looking like in five years? Are there any barriers to overcome before reaching this goal?
I think we have already overcome the biggest barrier so far – getting the method into the mainstream and having people work with it. I believe there are unlimited possibilities and opportunities to come over the next five years, particularly when integrating glycan imaging into all kinds of workflows.
New instrumentation will continue to be released, such as the MALDI-2 platform and improved ion mobility platforms. Glycan imaging is ideal for use in these workflows and with this type of instrumentation.
The other avenues are related to the enzymatic methods we have developed, such as those working with PNGase. We have been adapting these methods to other glycan targets in the glycocalyx, whether these are glycosaminoglycans, O-glycans, glycosphingolipids.
As these glycans are released from a protein, I think these methods are increasingly moving toward glycopeptide analysis, where we investigate the glycan and the protein carrier using the same assay. Being able to do glycopeptide imaging on the tissue would be a significant advance.
Additionally, with all the new multimodal types of analyses being developed, glycans fit beautifully into these spaces, whether targeting the single-cell space, or on the other end of the spectrum, the clinical imaging space.
Image Credit: BAIVECTOR/Shutterstock.com
How was the method developed?
The method has a fascinating history that involves my collaborators and colleagues, including Peggi Angel and Anand Mehta. It started around 2011 when Anand and I were at a review meeting for NCI.
I was getting the Solarix installed here at MUSC, having moved here around six months earlier. Anand had just created a new enzyme offering improved activity and stability – the PNGase Prime that we use now.
In 2012, we decided to look at what would happen if we sprayed this on tissue, and we achieved some initial results. By 2013, it was working on formalin fixed tissues.
In 2015, Peggy Angel joined MUSC, and she brought with her an abundance of experience and expertise in assay development, QC protocols and instrumentation. She worked with us to optimize the assay, making it robust, reproducible and feasible to export to other labs.
In 2018, Anand came to MUSC, and we have all been working together ever since, developing the assay for use not only on tissues but also for use with antibody arrays, serum assays and everything else we could apply it to.
In 2019 we formed the company GlycoPath to commercialize the assay, and we are also involved in another company called N-Zyme Scientifics that sells the enzymes that we spray on tissues.
About Bruker Daltonics

Discover new ways to apply mass spectrometry to today’s most pressing analytical challenges. Innovations such as Trapped Ion Mobility (TIMS), smartbeam and scanning lasers for MALDI-MS Imaging that deliver true pixel fidelity, and eXtreme Resolution FTMS (XR) technology capable to reveal Isotopic Fine Structure (IFS) signatures are pushing scientific exploration to new heights. Bruker's mass spectrometry solutions enable scientists to make breakthrough discoveries and gain deeper insights.
Sponsored Content Policy: News-Medical.net publishes articles and related content that may be derived from sources where we have existing commercial relationships, provided such content adds value to the core editorial ethos of News-Medical.Net which is to educate and inform site visitors interested in medical research, science, medical devices and treatments.
Bruker Daltonics
Source: Read Full Article