Study reveals new therapeutic target for aggressive type of rhabdomyosarcoma
To find new treatment approaches for childhood cancer, scientists at St. Jude Children’s Research Hospital are digging deep into disease biology to target a process long considered “undruggable.” The approach revealed a new strategy for treatment of an aggressive form of rhabdomyosarcoma. The findings were published today in Science Translational Medicine.
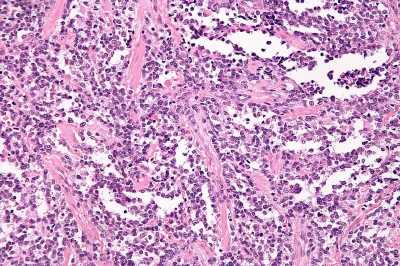
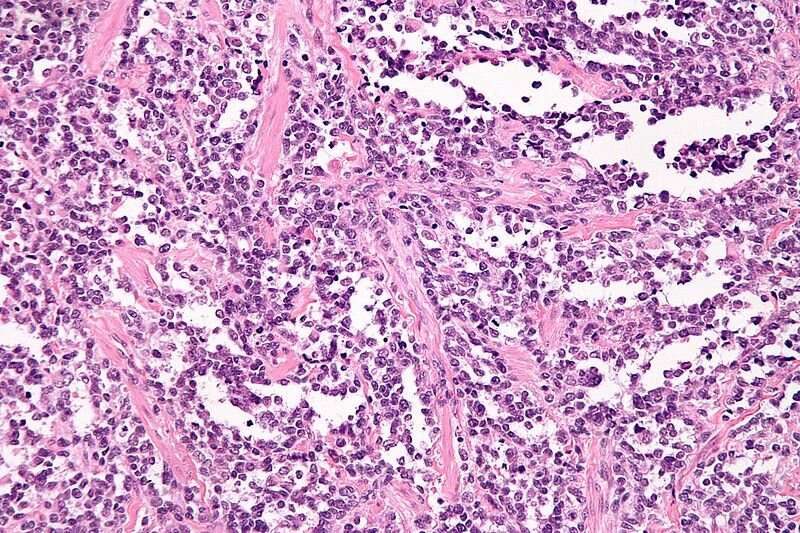
The strategy involves targeting a class of proteins called KDM4 for treatment of alveolar rhabdomyosarcoma driven by PAX3-FOXO1 gene fusions. Rhabdomyosarcoma is a type of cancerous tumor that arises in soft tissue, such as muscles. Soft tissue sarcomas comprise 7–8% of all childhood cancers. There are two types of rhabdomyosarcomas: embryonal and alveolar. The alveolar type occurs in children of all ages and often affects the large muscles of the arms, legs and trunk.
When a piece of one gene abnormally attaches to another, a gene fusion occurs. Together, these genetic pieces encode a fusion oncoprotein, which is a protein that plays a role in driving cancer. Alveolar rhabdomyosarcoma that contains the PAX3-FOXO1 fusion is more aggressive, has a higher rate of metastasis and poorer prognosis than cancers without the fusion.
“Rhabdomyosarcoma driven by this fusion is a dangerous disease that is very challenging to cure,” said corresponding author Jun Yang, M.D., Ph.D., St. Jude Department of Surgery. “It has few genetic mutations driving it, with limited treatment options for the fusion-positive version. By looking at a class of proteins that remove methylation marks from histones, we were able to identify a promising target that has been unappreciated until now. When combined with the standard of care, we saw a complete response in our models, which were often very resistant to chemotherapy alone.”
Targeting transcription
Transcription factors are proteins involved in the process of “transcribing” or converting the information in DNA into RNA. Transcription is an essential biological process because the RNA copy of a gene’s DNA sequence is used to make proteins. Transcription is normally a highly regulated process, but in cancer cells, it can be dysregulated. This dysregulation leads cancer cells to become dependent on abnormal proteins or factors involved in the process.
Core regulatory circuitry (CRC) refers to a set of transcription factors that establish and maintain cell identity (what kind of cell it is and how it functions). The PAX3-FOXO1 fusion is a genetic abnormality affecting transcription factors that play an essential role in constructing a CRC network for rhabdomyosarcoma.
“These transcription factors are really hard to target because they lack a binding pocket, so it is hard to develop any drug that can bind to them,” said co-first author Shivendra Singh, Ph.D., St. Jude Department of Surgery. “Cancer cells rely on these transcription factors and their CRC regulatory network. By targeting protein partners of the CRC, in this case KDM4B, we found you could collapse the network, effectively treating cancer.”
To study the PAX3-FOXO1 fusion and tease out the roles of different parts of the network, researchers conducted sophisticated analysis including RNA-seq, CUT&TAG and ATAC-seq. Through these efforts, they narrowed in on KDM4B, revealing that it is an important node in the CRC of alveolar rhabdomyosarcoma driven by the fusion oncogene.
“This study has been a very long journey, to understand the mechanisms behind why inhibiting KDM4 appears so successful in this subtype of rhabdomyosarcoma,” said co-first author Hongjian Jin, Ph.D., St. Jude Center for Applied Bioinformatics. “We were able to trace the important connections between KDM4 and the core regulatory circuitry of this cancer.”
A novel treatment strategy
Transcription factors are historically difficult to develop treatments against. However, their interaction with other proteins provides an opportunity to target their protein partners to disrupt their activity.
Using genetic methods and a compound that inhibits KDM4B in the lab, the researchers were able to substantially delay tumor growth. Combining KDM4B inhibition with currently used chemotherapy regimens caused tumors to shrink in preclinical xenograft models of the disease.
“We looked for epigenetic upstream regulators that can regulate these transcription factors and identified KDM4 specifically as one of these regulators, which is in itself novel,” said co-first author Ahmed Abu-Zaid, St. Jude Department of Surgery. “We also tested a targeted therapy in this cancer model, in combination with chemotherapy, which demonstrated a very effective anti-cancer effect. KDM4 inhibition has not been tried in this disease, so that is also exciting.”
Source: Read Full Article