Reducing drug overdoses by improving access to safe treatment
Layered over the pandemic in 2021 was an epidemic. Toxic drug overdoses in Canada spiked that year, with almost 8,000 reported deaths from opioid overdoses alone. In British Columbia, 2,264 people died that year of toxic drug overdoses.
“Continued reliance on traditional treatments such abstinence-based programs and opioid agonist therapy is insufficient to address the overdose crisis,” says Dr. Geoff Bardwell, assistant professor in the School of Public Health Sciences. He led a new study that examined facilitators and barriers to a novel intervention, a program that provides a regulated supply of opioids from a secure biometric machine dispenser.
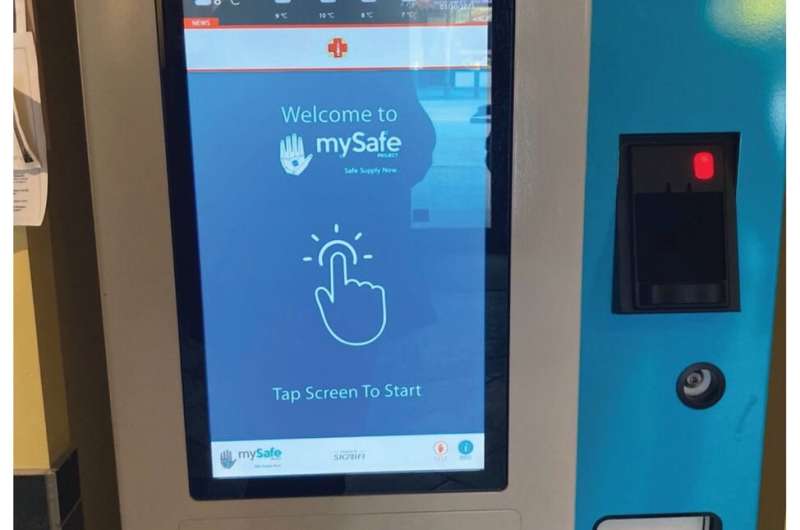
Called MySafe, the program was launched in Vancouver in 2021 with the aim of reducing drug overdoses. It allows eligible participants to scan their handprint to access daily prescribed hydromorphone tablets so that they need not seek illicit drugs. They can do so on their own time and without supervision. Eligible participants were people with opioid use disorders who purchased illicit fentanyl on the street and those who are generally considered at high risk for overdosing.
Bardwell says the study found that the program was successful in providing patients with a low-barrier and accessible means to receive a safer opioid supply. “This service delivery model may be able to circumvent barriers that exist at other safer supply programs,” he says. “For example, most other safer supply programs have set times that safer supplies can be accessed, and participants also report feeling embarrassed or ashamed when supervision is required.”
For the study, the researchers interviewed 46 participants in Vancouver who had been in the program for at least one month between November 2021 and April 2022. Fourteen identified as women, 13 as Indigenous and 32 as white, and they ranged in age between 25 and 68 years. Most lived in supportive housing.
The researchers found that all participants enjoyed the convenience and ease of accessing their safer supply from the machine, especially those dispensers that were accessible 24 hours per day. They also enjoyed increased privacy and autonomy and felt they were not being judged for taking these drugs.
They also reported that their increased independence allowed them to manage their medications for specific purposes. For example, some stockpiled the medication to be able to leave the city or go on vacation, or for when they would be unable to attend the program, limiting their need to seek illicit drugs.
However, 40 participants reported having technical issues with the machine almost once a month, usually frozen screens or error messages, sometimes leading to resort to the illicit market. Despite this and other barriers, most participants said they had reduced or eliminated their use of street-purchased drugs since enrollment, experienced fewer overdoses and increased health and well-being.
“When an individual purchases fentanyl on the street, it is not clear how strong the drugs will be, leading to unnecessary risk,” Bardwell says. “Identifying the facilitators and barriers to safer supply uptake is critical to preventing overdoses. Programs like MySafe provide a low barrier means of accessing prescribed opioids and show promise in addressing drug-related harms and improving health and social outcomes.”
The study, “Safer opioid supply via a biometric dispensing machine: a qualitative study of barriers, facilitators and associated outcomes,” is part of a larger, mixed-methods longitudinal evaluation of the MySpace program. It was co-authored by Geoff Bardwell, Andrew Ivsins, Manal Mansoor, Seonaid Nolan and Thomas Kerr and published in the Canadian Medical Association Journal (CMAJ).
More information:
Geoff Bardwell et al, Safer opioid supply via a biometric dispensing machine: a qualitative study of barriers, facilitators and associated outcomes, Canadian Medical Association Journal (2023). DOI: 10.1503/cmaj.221550
Journal information:
Canadian Medical Association Journal
Source: Read Full Article
