Move to Shorter Hypofractionated RT for High-Risk Prostate Cancer
SAN ANTONIO — Patients with high-risk prostate cancer can be safety treated with a shorter hypofractionated radiotherapy regimen without compromising overall and disease-free survival outcomes, suggest long-term results from a phase 3 trial from Canada.
The current standard radiotherapy regimen takes about 7–8 weeks, whereas the new regimen takes 5 weeks.
“That’s 3 weeks of not having to come to the clinic — the transportation, parking costs, and just the time it takes away from a person’s day-to-day life,” commented study presenter Tamim M. Niazi, MD, an associate professor of oncology at McGill University, Montreal, Quebec, Canada. “Our trial found no benefit to the extra 3 weeks.”‘
Niazi presented the results here at the American Society for Radiation Oncology (ASTRO) 2022 Annual Meeting on October 23.
Reacting to the presentation on Twitter, several oncologists wondered whether these new long-term results would lead to a shift in clinical practice.
Alison Tree, MD, PhD, consultant clinical oncologist, Royal Marsden Hospital, London, United Kingdom, asked: “Is this the end of 2 Gy/fraction for localized prostate cancer? I hope so.”
Martin Ma, MD, PhD, a radiation oncologist at UCLA Health, Los Angeles, California, said the results are “one more step in the right direction” for patients with high-risk prostate cancer. He too wondered whether it spells the “end of an era” for conventional regimens.
The trial compared the two regimens in 330 prostate cancer patients with high-risk disease characteristics who were also receiving androgen deprivation therapy (ADT).
After a median of 7 years of follow-up, the rates of overall, prostate cancer–specific, biochemical recurrence-free, and distant recurrence-free survival were virtually identical between the two treatment arms, with hazard ratios of around 1.
Moreover, rates of gastrointestinal and genitourinary toxicities, almost all of which were classified as grade 1 or 2, were broadly similar across the study, despite an initial peak of acute toxicities among patients given the hypofractionated regimen.
Hypofractionated radiotherapy is “as effective as conventional fractionation” and has “similar and acceptable toxicity,” Niazi concluded.
Moderate hypofractionated radiotherapy “should be considered as a new standard of care for high-risk prostate cancer patients considered for external-beam radiation therapy and long-term androgen deprivation therapy,” he added.
“Many of us already incorporate this into our clinical practice, but now we have the 7-year data to back us up,” commented study discussant Sophia C. Kamran, MD, assistant professor for radiation oncology, Harvard Medical School, Boston Massachusetts.
Kamran, who was not involved in the study, said the study “tells us that moderate hypofractionation for high-risk prostate cancer is safe, with comparable cancer control to standard fractionation.”
Nevertheless, there are “some open questions that remain,” Kamran said.
“Notably, treatment wasn’t shortened by much. It went from 7 weeks to about 5 weeks. The question is: If we further hyperfractionated or further shorten the treatment, does that lead to increased efficacy or increased toxicity?”
She also wondered whether radiation to the pelvic nodes, which was administered to all patients in the current trial, could be hypofractionated.
“Does that lead to increased efficacy or increased toxicity? Again, it remains to be seen and is being actively studied now” in other trials, she said.
Details of the Results
The majority of previous studies that investigated the use of moderate hypofractionated radiotherapy for patients with prostate cancer have focused on patients with low- or intermediate-risk disease, or they included mixed cohorts, Niazi commented.
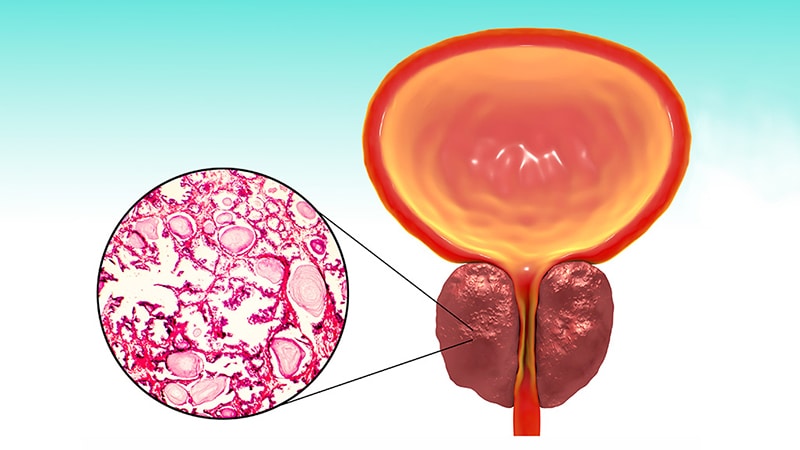
He emphasized that this trial focused on patients with high-risk prostate cancer, with stage T3a+ disease, a prostate-specific antigen (PSA) level of ≥20, and a Gleason score of 8–10. A total of 329 patients were recruited from 12 sites in Canada.
Between February 2012 and March 2015, they were randomly assigned in a 1:1 ratio to undergo standard fractionated radiotherapy or hypofractionated radiotherapy alongside ADT, which was taken for 28 months before, during, and after radiotherapy.
Standard radiotherapy consisted of 76 Gy delivered over 38 daily sessions, while hypofractionated radiotherapy involved 68 Gy delivered over 25 daily sessions. All patients also received radiotherapy to the pelvic nodes.
The median age of the patients was 72 years, and the two treatment arms were well balanced in terms of T stage, PSA level, Gleason score, and quality-of-life measures.
Niazi reported that after 7 years of follow-up, overall survival was virtually identical between the standard and hypofractionated radiotherapy arms, at 82.0% vs 81.7% (P = .76). There was also no appreciable difference in prostate cancer–specific mortality, at 96.4% vs 94.9% (P = .61).
Biochemical recurrence-free survival was also similar between the two arms, at 85.1% with standard radiotherapy and 87.4% among patients assigned to hypofractionated radiotherapy (P = .69), while rates of distant metastasis-free survival were 91.8% and 91.5%, respectively (P = .76).
Moreover, the hazard ratios for overall, prostate cancer–specific, biochemical recurrence-free, distant recurrence-free, and disease-free (combining biochemical and distant) survival were around 1.00 at 3, 5, and 7 years.
Regading safety, there was “minimal” grade 3 toxicity and “no grade 4 toxicity” in either treatment arm, Niazi reported.
The rate of grade ≥1 gastrointestinal-related acute toxicity was higher with hypofractionated than with standard radiotherapy, at an odds ratio of 1.76 (P = .016), as was the rate of grade ≥2 toxicity, at an odds ratio of 1.92 (P = .031).
Rates of grade ≥1 and grade ≥2 genitourinary-related acute toxicity were also numerically higher with hypofractionated radiotherapy, but the differences did not reach statistical significance.
Despite the initial peaks of gastrointestinal and genitourinary acute toxicity being higher with hypofractionated radiotherapy, they plateaued after around 8 months and approached the rates seen with standard radiotherapy, Niazi reported.
Late toxicities, whether gastrointestinal or genitourinary, were again almost exclusively of grade 1 or 2, and there were no significant differences in rates between the two treatment arms.
Niazi said that there are two potential future directions for this research: one is to further explore reducing the fractions to as few as five treatments, an approach known as ultra-hypofractionation; the other involves intensifying the hormonal therapy.
“We know the reason why patients unfortunately die of their cancer is because of metastasis, and the only way to reduce the rate of metastasis is to intensify systemic therapy,” he commented.
The study was supported by Sanofi Canada. Niazi has relationships with AbbVie, Astellas, Bayer, Janssen, Amgen, Sanofi, AstraZeneca, TerSera, Knight Therapeutics, Paladin, Watson, Merck, and Ferring. Kamran’s spouse is an employee of Sanofi.
American Society for Radiation Oncology (ASTRO) 2022 Annual Meeting: Abstract 4. Presented October 23.
For more news, follow Medscape on Facebook, Twitter, Instagram, and YouTube.
Source: Read Full Article