Fertility Doctors, IVF Families, Post-Roe: ‘We’re Anxious’
Married for nearly 5 years, Jessica King, 34, and her wife, Sarah, agreed on some things right from the start. “We always knew kids were in the equation,” Jessica says.
Now, Jessica is nearly 20 weeks pregnant, thanks to in vitro fertilization, or IVF. They did “reciprocal” IVF, with Sarah’s egg mixed with donor sperm and the embryo transferred into Jessica. “We’re excited—and terrified,” Jessica says.
But that terror goes beyond the typical concerns of excess weight gain and long labors. They live in Missouri, one of 13 states with so-called trigger laws that went into effect after the Supreme Court overturned Roe v. Wade and the constitutional right to abortion, giving states the power to regulate it. States with trigger laws either banned abortion immediately or within a specified time frame after the ruling. In all, 26 states are expected to have abortion restrictions.
Missouri now allows abortion only for medical emergencies. If her upcoming ultrasound shows serious issues, Jessica says they could easily travel to another state and pay for an abortion. She realizes not everyone can.
However, the concern about trigger laws goes well beyond abortion. Many experts worry about the “spill-over” effects the abortion laws — both the existing ones and future proposals — may have on fertility care and treatments.
“Personhood” Laws Drive the Concern
“The current trigger laws on the books are not impacting people’s access to IVF,” says Barbara Collura, president and CEO of RESOLVE, an advocacy group for those with fertility issues. “What we are concerned about is they will come back and make them stronger.”
The chief concern for reproductive rights advocates is so-called “personhood” legislation. According to the Guttmacher Institute, at least 6 bills about personhood have been introduced in five states, including Iowa, Oklahoma, South Carolina, Vermont and West Virginia. One of the two Oklahoma bills has gone the farthest, passed by one chamber.
Since the Guttmacher report, Ohio introduced its own personhood legislation July 11, recognizing the personhood of an unborn person from conception.
Personhood legislation defines a fertilized egg or embryo as a legal human entity, says Sean Tipton, chief policy and advocacy officer for the Washington, D.C.-based American Society of Reproductive Medicine, a nonprofit advocacy group.
“If the legal status of fertilized eggs or early embryos is codified, in vitro fertilization procedures may become legally risky for patients, physicians and staff,” Tipton wrote in late June in
Contemporary OB/GYN Journal. The American Society for Reproductive Medicine has posted a report on state abortion trigger laws and their potential implications for reproductive medicine. Of the 13 with trigger laws in effect, the report found concern about the potential effect on IVF only with Utah’s.
“Safe” States?
Even in states without trigger laws or personhood bills, IVF patients say they are anxious about how the Supreme Court ruling may ultimately affect care. Thanks to IVF, Shelly Battista and her husband Robert are expecting twins in December, little sisters to their daughter Emilia, who is 2-and-a-half.
They live in Illinois, where abortion is legal. “Even though we are safe now, I think the overturning of Roe has made it clear to all of us that none of our freedoms are safe, especially reproductive rights,” Shelly says.
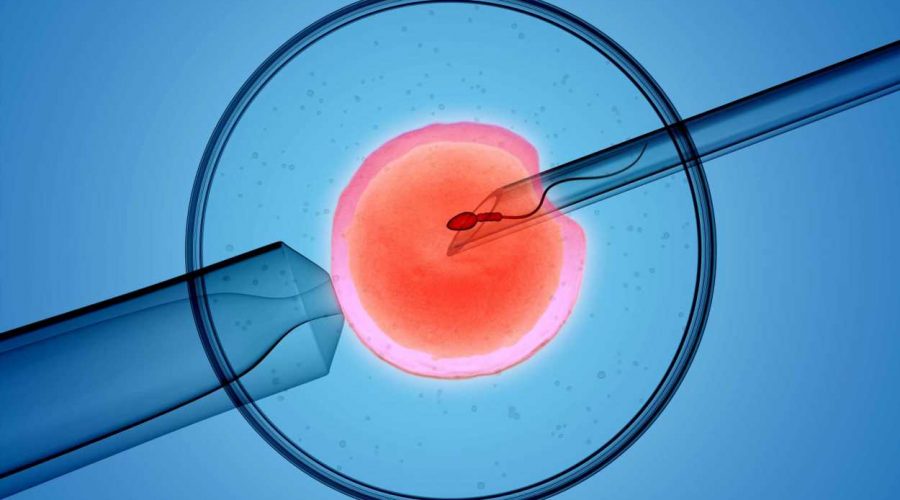
About 1 in 8 U.S. couples are infertile, according to RESOLVE, In 2019, 2% of all babies born in the U.S., or about 78,000 infants, were conceived with the use of assisted reproductive technologies, according to the CDC. The most common assisted reproductive technology is IVF, in which the sperm fertilizes the egg outside the body and an embryo is then transferred.. The standard of practice is to transfer a single embryo, freezing others for future use.
Trigger State Doctors Weigh In
Some fertility doctors in those “trigger” states are keeping a close eye on proposed legislation and talking to legislators for interpretation of current and proposed laws.
Eli Reshef, MD, a reproductive endocrinologist and fertility specialist at Bennett Fertility Institute in Oklahoma City, notes that his state has “the strictest abortion law in the land.” The law prohibits all abortions with few exceptions, such as the removal of an ectopic pregnancy (when a fertilized egg implants outside the uterus, such as in the fallopian tubes).
While IVF will not be affected for now, he worries that the Oklahoma law allows a private citizen to sue a health care provider that they feel is performing abortion./ The Oklahoma law, leaves interpretation of abortion up to the general public, who may be unfamiliar with the language of the law, House Bill 4327.
Dean Moutos, MD, a reproductive endocrinologist and medical director of Arkansas Fertility and Gynecology in Little Rock, says his state’s current trigger law should not affect IVF. “When you read the bill, it says abortion means to terminate the pregnancy of a woman.” Still, he says, “we are concerned about what might happen in the future” and the possibility that some legislators may interpret that differently.
A Minority Approach
John David Gordon, MD, a reproductive endocrinologist and medical director of Southeastern Fertility Center for Fertility and Reproductive Surgery in Knoxville, TN, is also in a trigger state. However, it’s not likely any personhood laws would affect his practice.
That’s because his center, which he acknowledges is clearly in the minority, only performs natural cycle IVF, which usually results in a single egg, or “mini stim IVF,” which usually results in 3 to 8 eggs in order to limit the number that may be potentially fertilized. Often, he says, patients choose to freeze unfertilized eggs (alone) to avoid creating an excessive number of embryos. He has a “no discard” program, with any viable embryos frozen or transferred. Abandoned embryos are donated to others.
“This may work for young women,” says Marcelle Cedars, MD, director of reproductive endocrinology at the University of California San Francisco, and president of the American Society of Reproductive Medicine. However, she says it will be very inefficient for older patients, since they have a higher percentage of abnormal eggs.
Overall, that approach will also drive up costs, especially for older women, Cedars says. An average cycle of IVF costs $12,400, and most Americans’ insurance plans don’t cover IVF, according to Tipton.
Top Concerns for IVF
“Personhood” legislation has the potential to upend many common IVF practices, experts say.
Of greatest concern to fertility practices are potential restrictions on the freezing or discarding of embryos, Cedars says. “This could have a critical impact on practicing the safest, most evidence-based medicine,” she says.
Most children born in the U.S. as a result of IVF procedures are born from frozen embryos, according to the Society for Assisted Reproductive Technology, an organization for reproductive specialists.
“The practice of IVF really requires that we generate more embryos than will be used in a given [IVF] cycle,” agrees Kara Goldman, MD, associate professor of obstetrics and gynecology and medical director of the fertility preservation program at Northwestern University Feinberg School of Medicine outside Chicago. She performed the embryo transfer for the Battistas.
In nature, she says, it’s known that only a small number of eggs will be competent to generate a baby. “We see the same thing in IVF.” In a single cycle, 20 eggs may be retrieved, but many fewer typically reach successful fertilization and are able to be implanted.
When patients have completed their family, unused embryos are donated to research, donated for adoption or destroyed. If embryo destruction is outlawed, Goldman says, it will have serious ramifications for the practice of IVF.
And if personhood legislation prohibits destroying any embryos, others wonder: would a lab technician who accidentally dropped and destroyed an embryo be subject to charges? If laws prohibit destruction of embryos, others wonder if will families be forced to pay the embryo storage fees, generally $500 to $1,000 a year, in perpetuity.
If an embryo is declared a person, it could also affect a practice called preimplantation genetic testing, or PGT. In PGT, cells are retrieved from an embryo and checked for genetic disorders such as sickle cell anemia and cystic fibrosis, with some parents choosing to discard embryos that are found to be affected.
Some potential parents choose this testing because they know they are carriers for genetic diseases that are serious and even incompatible with life, says Art Caplan, PhD, head of the division of medical ethics at the New York University Grossman School of Medicine. They may choose to discard embryos that show evidence of the diseases.
Also under fire could be “selective reduction,” reducing multiple fetuses to a single or twin, to reduce risks to babies and mother.
Caplan predicts if states have many restrictions, some providers will adopt the attitude that “if no one reports, it did not happen.” And those prospective parents with the means, he says, will go to court and fight restrictions. “When they do it, they are saying, ‘You say you are pro-life; I’m trying to have a child. What are you doing getting in my way?'”
IVF Families: Tough Decisions, Emotional Times
The Battistas, of Illinois, have had an especially rough road. Shelly was diagnosed with a fast-growing breast cancer in 2020, when Emilia was just an infant. Warned that the chemotherapy she needed would suppress her ovaries, Shelly underwent egg retrieval before starting the cancer treatment.
She opted to have a double mastectomy and her ovaries removed after learning she carried the BRCA1 genetic mutation, boosting the risk of both breast and ovarian cancer.
Once she was cancer-free, she was cleared to start IVF. The first two embryo transfers failed. The third transfer, of a single embryo, was successful. But it split, a rare occurrence, producing two embryos. “It was a big shock, but in the best way,” she says about learning they were having twins. “Now we are over the moon.”
Five frozen embryos remain. At the start, the Battistas decided to discard unused embryos. She and Robert are discussing what to do next. If they decide they are done building their family after the twins’ birth, she wonders, “do we need to discard our [other] embryos before that becomes something that isn’t eligible [possible] for us any longer?” She. doesn’t want to be rushed into that decision, however, especially with her medical history.
Jessica King and Sarah have 20 more embryos.
The couple had decided to donate unused embryos for research, when the time comes, and for different reasons. Her wife’s decision is based on her belief in science, while Jessica cites her faith. “As a Jew, it is part of our faith, that we should be doing everything we can to advance humanity,” she says.
In the midst of all the uncertainty, Jessica says, only half-jokingly, that she is tempted to claim the frozen embryos as dependents. “If you are truly going to claim these are precious human lives, you should be giving me all the benefits from having children,” she says.
Shelly knows that having one daughter, with two more on the way, affects her thinking about the court’s ruling. “My overall wish would be that Roe v.. Wade is reinstated, and my daughters have the same rights and options that I have…or I did have until my current 36 years of life.”
Sources
Shelly Battista, 36, mother and IVF patient, Chicago.
Barbara Collura, president and CEO, Resolve, The National Fertility Association, McLean,VA.
Sean Tipton, chief policy and advocacy officer, American Society for Reproductive Medicine, Washington, D.C.
Contemporary OB/GYN Journal: “Not just abortion: How the demise of Roe v. Wade may impact fertility care.”
Eli Reshef, MD, reproductive endocrinologist, fertility specialists, Bennett Fertility Institute, Oklahoma City, OK.
Dean Moutos, MD, reproductive endocrinologist and medical director, Arkansas Fertility & Gynecology, Little Rock, AR.
John David Gordon, MD, reproductive endocrinologist and medical director, Southeastern Fertility Center for Fertility and Reproductive Surgery, Knoxville, TN.
Marcelle Cedars, MD, director of reproductive endocrinology, University of California San Francisco and president, American Society for Reproductive Medicine.
Art Caplan, PhD, head, division of medical ethics, NYU Grossman School of Medicine, New York.
Kara Goldman, MD, associate professor of obstetrics and medical director, fertility preservation program, Northwestern University Feinberg School of Medicine, Chicago.
Jessica King, architect and IVF patient, St. Louis, MO.
Society for Assisted Reproductive Technology, Birmingham, AL.
Resolve: “Opposing Personhood.”
Guttmacher Institute: “13 States Have Abortion Bans—Here’s What Happens When Roe Is Overturned,” “State Legislation Tracker.”
CDC: “Assisted Reproductive Technology (ART).”
ASRM: “State abortion trigger laws.”
Ohio House bill (HB) 704.
Source: Read Full Article