COVID-19 mortality strongly predicted by autoimmunity to type I interferons and advancing age
In a recent study published in the journal PNAS, researchers estimated the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection fatality rate (IFR) and relative risk of death (RRD) among subjects across ages. Study participants were either carriers of autoantibodies (auto-Abs) which neutralized low concentrations (100 pg/mL), or high concentrations (10 ng/mL) of type I interferons (IFNs) such as FN-α, IFN-β, and IFN- ω or non-carriers.
Studies have reported that pre-existing auto-Abs neutralizing type I IFNs are strong predictors of life-threatening coronavirus disease 2019 (COVID-19) pneumonia. Furthermore, the auto-Abs prevalence and the COVID-19 mortality risks are higher among males and increase with advancing age. Therefore, it is vital to quantify the impact of such auto-Abs on COVID-19-associated deaths by sex and age.
 Study: The risk of COVID-19 death is much greater and age-dependent with type I IFN autoantibodies. Image Credit: NIAID
Study: The risk of COVID-19 death is much greater and age-dependent with type I IFN autoantibodies. Image Credit: NIAID
About the study
In the present study, researchers estimated the COVID-19 IFR and RRD among deceased COVID-19 patients and the general public who were either carriers of type I IFN-neutralizing auto-Abs or non-carriers.
The study comprised 1,261 unvaccinated deceased COVID-19 patients and 34,159 subjects of the general public who were sampled before the COVID-19 pandemic. The study population was aged between 20 years and 99 years. The deceased COVID-19 patients died from COVID-19 pneumonia.
For auto-Abs that neutralized low concentrations of IFN-ω and/or IFN-α2, 1,121 deceased COVID-19 patients and 10,778 subjects from the general public were analyzed. Auto-Abs that neutralized high concentrations of IFN-ω and/or IFN-α2 were assessed among 1,094 deceased COVID-19 patients, and 34,159 individuals from the general public. Auto-Abs that neutralized high concentrations of IFN-β among 636 deceased COVID-19 patients and 9,126 subjects from the general public were also assessed.
The RRD of subjects carrying auto-Abs neutralizing type I IFNs relative to non-carriers was estimated using Firth's logistic regression model. The odds ratios (ORs) obtained using logistic regression were approximated to the relative risks (RRs). In addition to the overall IFRs, IFRAAB were calculated based on Bayes' theorem. The population attributable fraction (PAF) was also assessed to evaluate the proportion of COVID-19 mortality attributable to auto-Abs.
Results
The RRD associated with any auto-Abs combination was more significant among subjects aged below 70 years. For auto-Abs that neutralized either IFN-ω or IFN-α2, the RRDs were 17 and 5.8 for subjects aged below and above 70 years, respectively. On the other hand, for auto-Abs that neutralize IFN-ω and IFN-α2, the corresponding RRDs were 188.3 and 7.2, respectively.
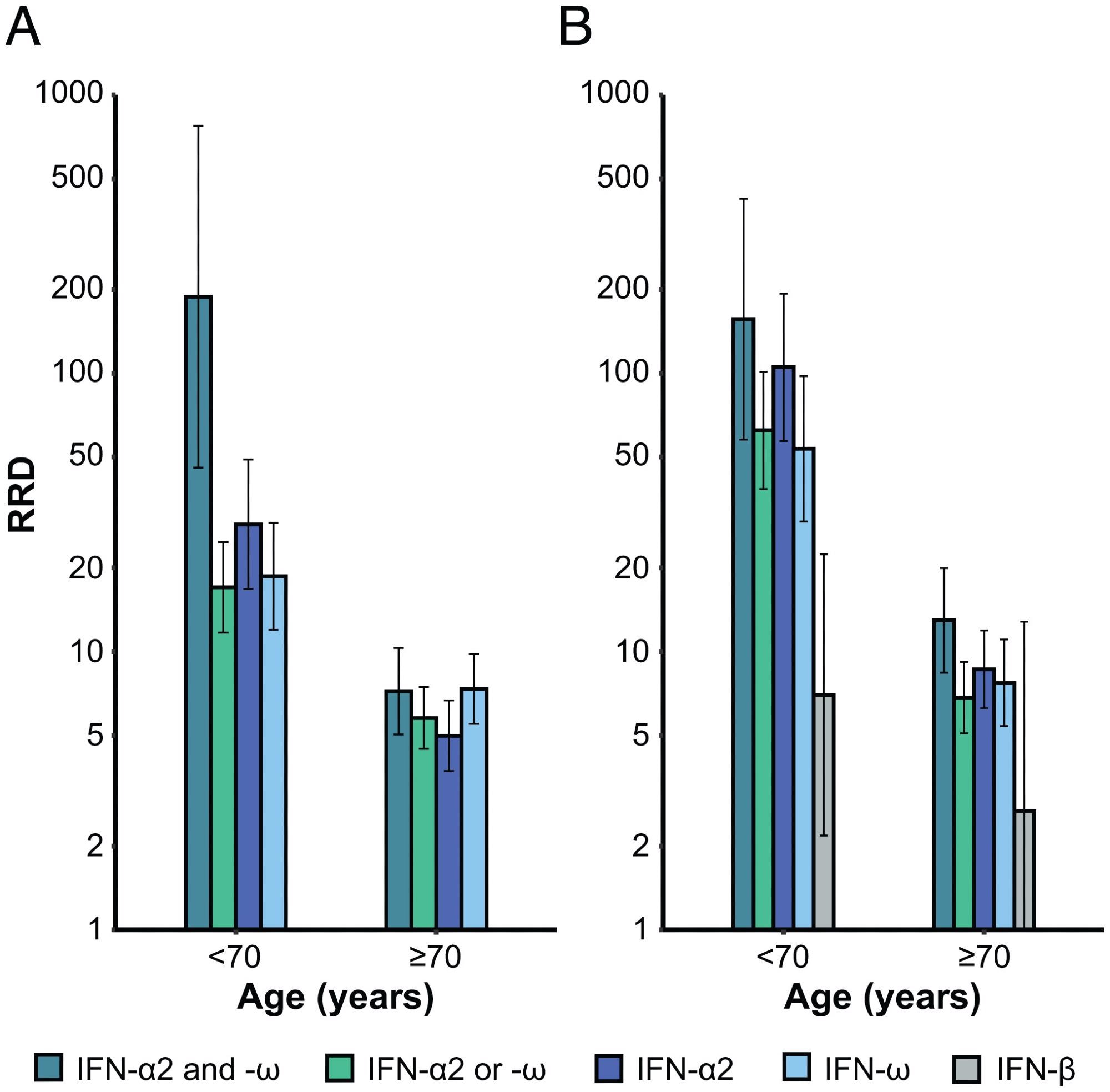 RRDs for individuals with auto-Abs neutralizing different combinations of type I IFNs relative to individuals without such auto-Abs, by age. RRDs are displayed on a logarithmic scale for individuals under and over 70 y of age with (A) auto-Abs neutralizing low concentrations of IFN-α2 and IFN-ω, IFN-α2 or IFN-ω, IFN-α2, and IFN-ω and (B) auto-Abs neutralizing high concentrations of IFN-α2 and IFN-ω, IFN-α2 or IFN-ω, IFN-α2, IFN-ω, and IFN-β, relative to individuals without such combinations of auto-Abs. Vertical bars represent the 95% CI.
RRDs for individuals with auto-Abs neutralizing different combinations of type I IFNs relative to individuals without such auto-Abs, by age. RRDs are displayed on a logarithmic scale for individuals under and over 70 y of age with (A) auto-Abs neutralizing low concentrations of IFN-α2 and IFN-ω, IFN-α2 or IFN-ω, IFN-α2, and IFN-ω and (B) auto-Abs neutralizing high concentrations of IFN-α2 and IFN-ω, IFN-α2 or IFN-ω, IFN-α2, IFN-ω, and IFN-β, relative to individuals without such combinations of auto-Abs. Vertical bars represent the 95% CI.
Contrastingly, IFRs were higher with advancing age, and ranged from 0.17% to 26.7% among subjects aged below 40 years and above 80 years, for auto-Abs neutralizing IFN-ω or IFN-α2. The IFRs ranged from 0.84% to 40.5% for auto-Abs, which neutralized IFN-ω and IFN-α2.
For all auto-Abs combinations, the IFRAAB was much higher than the overall IFR among carriers of auto-Abs, neutralizing low concentrations of IFN-ω or IFN-α2. The IFRAAB values exceeded 1% among subjects aged above 40 years and 10% among those aged above 60 years. The highest IFRAAB of 40.5% was observed for carriers of auto-Abs neutralizing IFN-ω and IFN-α2 who were aged above 80 years.
Of note, the IFRAAB values were higher among males compared to females by 2.7-fold, and 5-fold, especially among subjects carrying auto-Abs which neutralized low concentrations and high concentrations of IFN-ω and IFN-α2, respectively. The PAFs for auto-Abs neutralizing low and high concentrations of type I IFNs were found to be very close to the prevalence of auto-Abs among deceased COVID-19 patients.
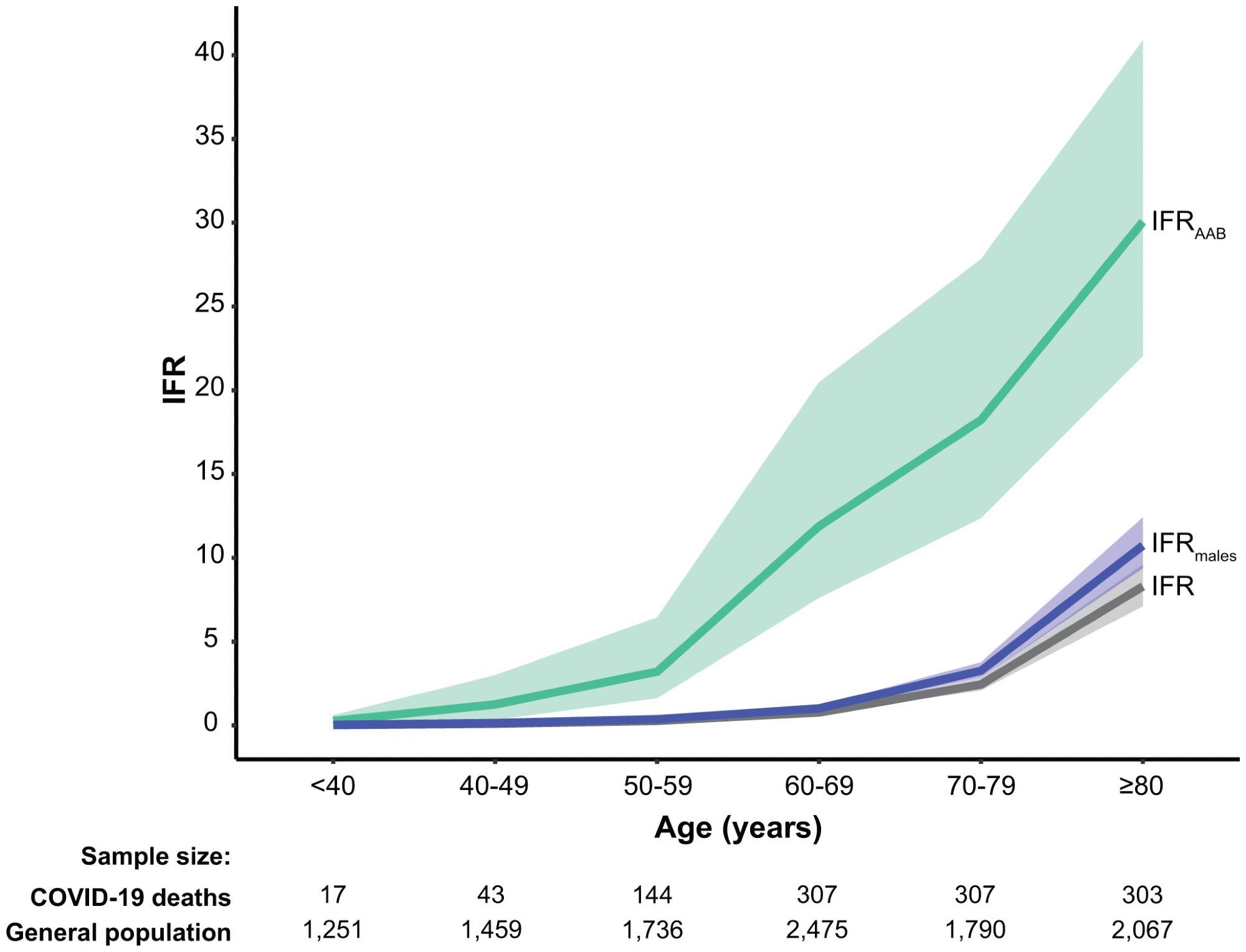 SARS-CoV-2 IFRs by age. IFRs are provided for the general population for both sexes (gray) and for males only (blue), from the data of O’Driscoll et al.; IFRAAB (green) are shown for individuals carrying auto-Abs neutralizing low concentrations of IFN-α2 or IFN-ω. Auto-Abs against type I IFNs are associated with high RRDs and strongly increase the IFR, to a much greater extent than being male, and, by inference, than other common classical risk factors providing ORs of death similar to that for being male (around two), such as certain comorbid conditions, or the most significant common genetic variant on chromosome 3.
SARS-CoV-2 IFRs by age. IFRs are provided for the general population for both sexes (gray) and for males only (blue), from the data of O’Driscoll et al.; IFRAAB (green) are shown for individuals carrying auto-Abs neutralizing low concentrations of IFN-α2 or IFN-ω. Auto-Abs against type I IFNs are associated with high RRDs and strongly increase the IFR, to a much greater extent than being male, and, by inference, than other common classical risk factors providing ORs of death similar to that for being male (around two), such as certain comorbid conditions, or the most significant common genetic variant on chromosome 3.
Type I IFN neutralizing auto-Abs increased IFRs and were associated with high RRDs, particularly those which neutralized both IFN-ω and IFN-α2. Notably, IFRs increased significantly with age and male sex, whereas RRDs decrease with age and did not significantly vary with sex.
Conclusions
Overall, the study findings showed that the male sex, increased age, and the presence of auto-Abs against type I IFNs strongly increased the SARS-CoV-2 IFR among COVID-19 deceased patients and the general public.
Type I IFN immunity is necessary for protective immunity against SARS-CoV-2 infections. Auto-Abs against type I IFNs are strong and commonly used predictors of life-threatening COVID-19. Therefore, testing for the Type I IFN neutralizing auto-Abs should be considered to assess the risk of COVID-19 mortality among COVID-19 patients and the general public.
- The risk of COVID-19 death is much greater and age-dependent with type I IFN autoantibodies.Jeremy Manry, Paul Bastard, Adrian Gervais,and Aurélie Cobat. PNAS 2022 Vol. 119 No. 21 e2200413119, DOI: https://doi.org/10.1073/pnas.2200413119, https://www.pnas.org/doi/10.1073/pnas.2200413119
Posted in: Medical Research News | Disease/Infection News
Tags: Autoantibodies, Autoimmunity, Chromosome, Chromosome 3, Coronavirus, Coronavirus Disease COVID-19, Genetic, immunity, Interferons, Mortality, Pandemic, Pneumonia, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Syndrome

Written by
Pooja Toshniwal Paharia
Dr. based clinical-radiological diagnosis and management of oral lesions and conditions and associated maxillofacial disorders.
Source: Read Full Article
