Convalescent plasma therapy provides limited success in treating COVID-19
Convalescent plasma therapy was one of the first treatments available in the battle against COVID-19. But since the therapy’s emergency use authorization by the Food and Drug Administration in August 2020, its supposed benefits have been met with scrutiny by some researchers.
To investigate the success of convalescent plasma therapy in reducing the severity and mortality of COVID-19, a team of researchers from seven institutions came together, including Alessandro Santin, MD, professor of obstetrics, gynecology, and reproductive sciences, and Mahalia Desruisseaux, MD, associate professor of internal medicine (infectious disease), who led the portion of the clinical trial done at Yale School of Medicine. While the therapy, the team found, provided no improvement in the overall survival of COVID-19 patients says Santin, it shouldn’t be ruled out in early pandemic cases where no other treatment options are available. The team reported their results in JAMA Internal Medicine on December 13.
“This is one of the largest double-blind prospective randomized studies ever done on COVID-19 for patients with severe disease,” says Santin.
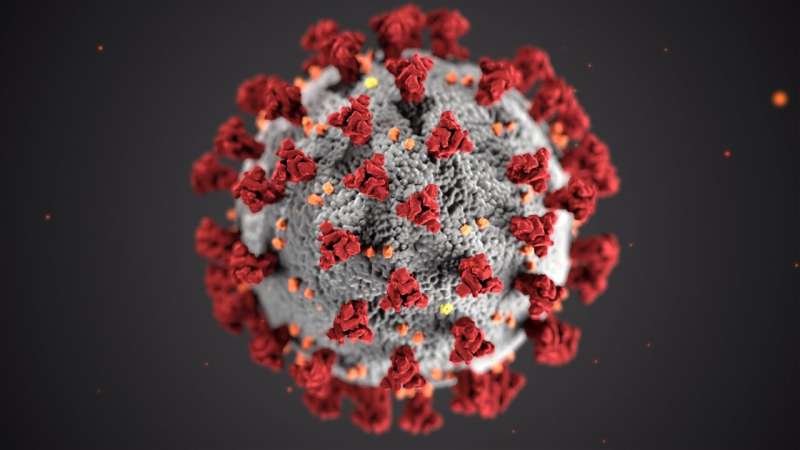
Convalescent plasma therapy involves health professionals collecting antibodies that fight diseases such as COVID-19 through extracting blood plasma from donors who have survived the disease. By providing patients with these borrowed antibodies that are specific against the variant spreading in the population at a specific time point, the goal of the therapy is to give sufferers of the disease what scientists refer to as “passive immunity.” The use of convalescent plasma therapy dates back to the 1918 Spanish flu and has been used over the last century to fight outbreaks including the smaller SARS-CoV-1 outbreak in 2003.
“The bottom line is that the evidence showed during both the Spanish flu 100 years ago and SARS-COV-1 that fewer people were dying after being treated with convalescent plasma,” says Santin.
The clinical trial, known as CONTAIN COVID-19, began in April 2020, during the early days of the pandemic in the United States. The study began by enrolling hospitalized COVID-19 adult patients in New York City, but would soon expand to include patients in 21 hospitals affiliated with seven centers across the country, including Yale School of Medicine. In total, 941 patients who had been hospitalized for less than three days or experienced symptoms for less than seven days were enrolled. Four hundred sixty-eight patients received the convalescent plasma therapy, while 473 patients were given an equivalent amount of saline.
Overall, the researchers found no significant difference in mortality rate between the treatment and placebo groups. At first, says Santin, this result was disappointing. However, when the researchers looked at the data from first three months of the trial, the patients in the treatment group did experience improvement compared to the control group. Santin says that the difference between the early months and the rest of the study is likely explained by the approval of new effective treatment options (ie, dexamethasone and/or remdesivir) after that time point.
“It’s important to note that when we started the trial, we had no other options for treating COVID-19,” says Santin. “But later on, when doctors started using corticosteroids, as well as remdesivir, the signal of activity we saw associated with convalescent plasma disappeared.”
When combined with other strategies, convalescent plasma therapy failed to provide a sufficient additional benefit. However, Santin says, the treatment should not be ruled out entirely as an effective treatment option since during the early months of the pandemic when other agents were not available, a signal of activity was detectable. In the right setting, there might be a place for the use of convalescent plasma early in future pandemics before a definitive treatment regimen is defined. And as new SARS-CoV-2 variants arise and become resistant to available vaccines or monoclonal antibodies, health care workers may need to turn back to convalescent plasma. Immunosuppressed patients such as cancer or transplant patients, who cannot produce sufficient antibodies on their own, may also continue to benefit from a passive immunity strategy.
Source: Read Full Article
