An artificial muscle to study Duchenne muscular dystrophy
Duchenne muscular dystrophy (DMD) is the most common muscular dystrophy diagnosed in childhood, with approximately 20,000 new cases reported each year. It is a progressive muscle disorder that results in the loss of muscle function, ultimately leading those affected to lose their independence and experience severe medical issues. The average life expectancy for individuals with DMD is around 30 years.
The cause of the disease is a mutation in the gene encoding dystrophin, a protein that cushions the impact of muscle contraction on the cell membrane. Due to the absence of dystrophin, muscle cells are prone to easy damage.
Currently, there is no cure for DMD, and one of the primary challenges that the research community faces is to develop artificial models capable of accurately replicating the damage found in patients’ muscles. This is essential for studying new treatments in the laboratory.
A study conducted by the Institute of Bioengineering of Catalonia (IBEC), published this week in the journal Biofabrication, describes the development of a 3D muscle model capable of replicating the damage found in the muscle tissue of individuals affected by Duchenne muscular dystrophy.
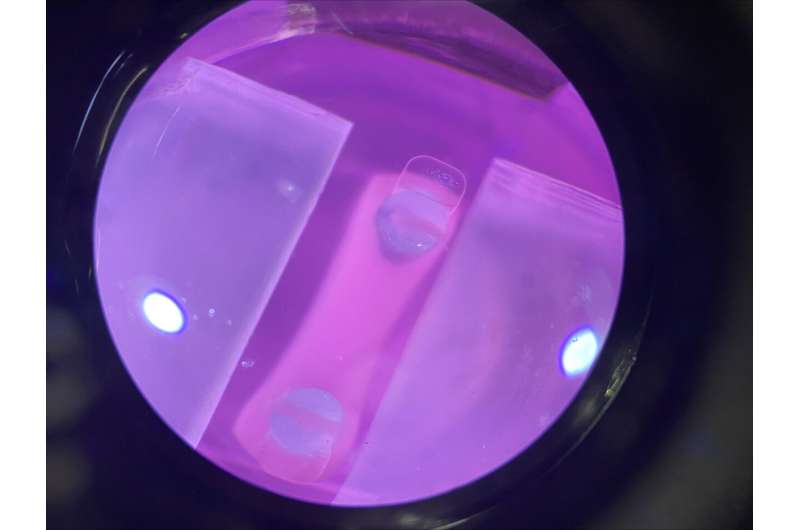
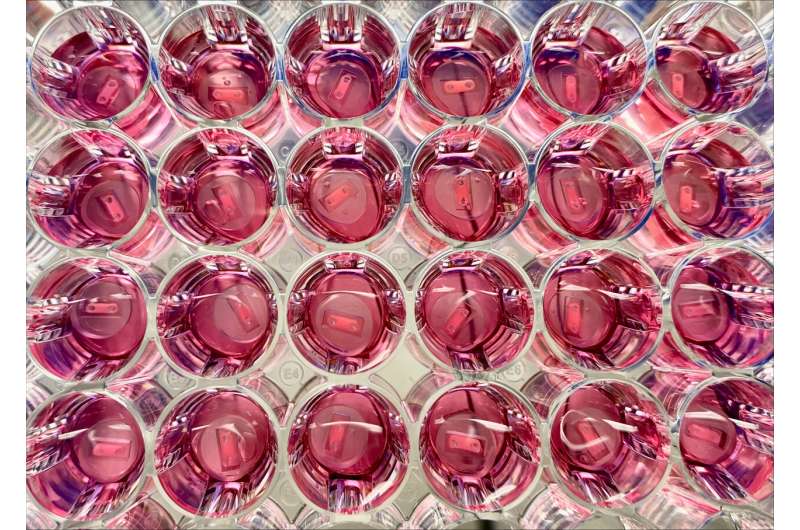
The system, created through tissue engineering using patient cells, includes muscle fibers that can contract when an electrical stimulus is applied. This is a crucial feature for establishing an artificial muscle model that enables preclinical studies of drugs for treating DMD
The work was led by Juanma Fernández Costa, a senior researcher at IBEC, with Ainoa Tejedera Villafranca, a Ph.D. student at IBEC, serving as the first author. Both of them are part of the Biosensors for Bioengineering group, which is led by ICREA research professor Javier Ramón Azcón.
“The novelty of this study lies in our attempt to model the primary cause of the disease, which is damage to the sarcolemma, the membrane of muscle cells. It was crucial for us to replicate this in the laboratory, and we have successfully accomplished it. This had not been done previously,” says Juanma Fernández.
“We worked for a long time on different protocols until we managed to make that damage appear in the cells of patients, but not in the control cells of people without Duchenne. It’s delicate because if you stimulate the muscle, you can also cause fiber breakage in healthy cells, just as it happens when we play sports and experience muscle soreness,” adds Ainoa Tejedera.
The goal of the researchers was to create a model that would enable them to determine whether drugs can reverse this cell damage. Rather than addressing the symptoms, which is the focus of palliative treatments, they aimed to target the root cause of the disease.
Although they have already tested some drugs using this model, they are working on developing an enhanced model called an organ-on-a-chip. It is a more advanced platform that incorporates sensors and a microfluidic system into the 3D muscle model. This will enable more efficient monitoring of cell damage and faster testing of various molecules or drugs.
More information:
Ainoa Tejedera-Villafranca et al, Mimicking sarcolemmal damage in vitro: a contractile 3D model of skeletal muscle for drug testing in Duchenne muscular dystrophy, Biofabrication (2023). DOI: 10.1088/1758-5090/acfb3d
Journal information:
Biofabrication
Source: Read Full Article
