A simple online calculator detects liver cirrhosis patients at high risk for clinical complications
Researchers at CeMM, the Medical University of Vienna (MedUni Vienna), and the Ludwig Boltzmann Institute for Rare and Undiagnosed Diseases (LBI-RUD) joined efforts to use their expertise in machine learning and management of patients with cirrhosis to develop a non-invasive algorithm that can help clinicians to identify patients with cirrhosis at highest risk for severe complications.
Cirrhosis develops in response to repeated injury to the liver, such as fatty liver disease or viral hepatitis. Initially, cirrhosis is mostly asymptomatic, thus, early identification of risk factors for severe complications represents an unmet clinical need.
There are two clinical stages of liver cirrhosis: compensated and decompensated. Patients with compensated liver cirrhosis have very few or even no symptoms. However, patients may progress decompensated cirrhosis, which occurs with severe complications such as internal (variceal) bleeding or by an accumulation of fluid in the abdomen (ascites) and may even lead to death.
Unfortunately, the measurement of the risk of decompensation in patients with compensated cirrhosis currently requires an invasive procedure. i.e., the measurement of the hepatic venous pressure gradient (HVPG). An elevated HVPG ≥10 mmHg is associated with a higher probability of complications. Patients with an even higher HVPG of ≥16 mmHg are at imminent risk for hepatic decompensation.
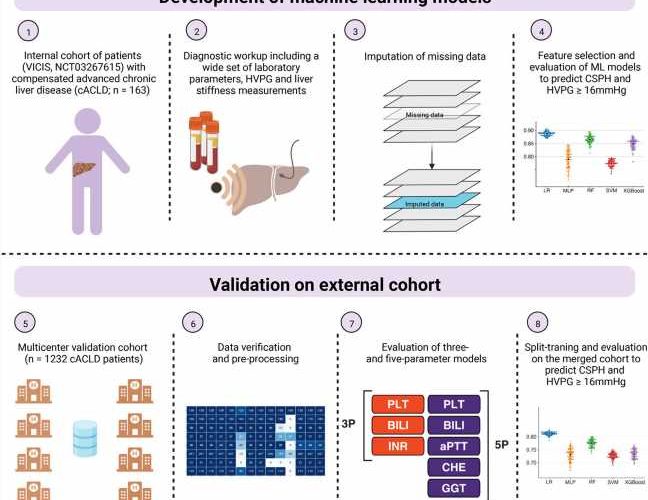
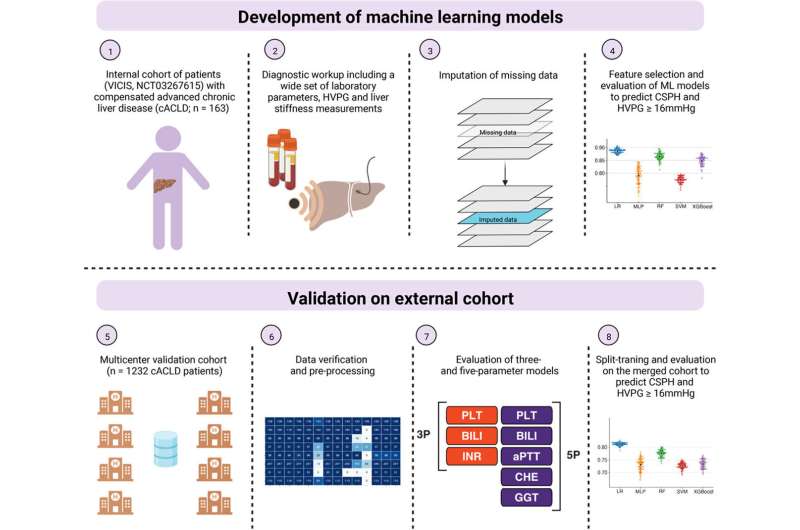
In a study by first authors Jiri Reinis from Stefan Kubicek’s group at CeMM and Oleksandr Petrenko from Thomas Reiberger’s group at MedUni Vienna, CeMM, and LBI-RUD, machine learning models were trained on blood test parameters obtained from patients with compensated cirrhosis to detect elevated levels of portal vein pressure, thereby identifying those at risk for developing clinical complications. The study is now published in the Journal of Hepatology.
Best clinical parameters for prediction
The key data sources used in the project were derived from the ongoing Vienna Cirrhosis Study, conducted at the Division of Gastroenterology and Hepatology of the MedUni Vienna at the Vienna General Hospital. For this study, HVPG measurements were performed in 163 compensated cirrhosis patients in whom blood samples were simultaneously obtained in order to determine a range of 124 biomarkers.
Out of the entire set of clinical variables, three and five optimal parameters for the detection of high-risk patients were computationally determined. In the VICIS patient cohort, the model performed excellently for the identification of patients with HVPG values of ≥10 mmHg and ≥16 mmHg, respectively.
Validation of the dataset
To assess the diagnostic power of the non-invasive models to predict complications, the researchers tested their non-invasive machine learning model on a combined cohort of 1,232 patients with compensated cirrhosis from 8 European clinical centers. The novel approach was confirmed to be of excellent diagnostic value in the overall cohort and importantly is based on 3 or 5 widely available laboratory parameters only, is non-invasive, and does not require dedicated and expensive equipment.
Project leader Thomas Reiberger explains that “while an HVPG measurement is still required for reliable identification of patients with clinically significant or severe portal hypertension, the novel approach could be applied for prioritization for treatment to prevent decompensation or for selection of patients for clinical trials. Due to its simplicity, the proposed methodology could be eventually employed during routine check-ups at little additional cost.”
Source: Read Full Article