The use of mammalian cell surface display for rapid characterization of SARS-CoV-2 variants
A research group from the U.S. demonstrated the practicality of a spike display system in order to accelerate vaccine design, but also to swiftly appraise the effects of mutations in emerging strains of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Their results are currently available on the bioRxiv* preprint server.
SARS-CoV-2, the causative agent of the ongoing coronavirus disease (COVID-19), uses its spike glycoprotein to interact with angiotensin-converting enzyme 2 (ACE2) in order to fuse cell membrane and viral envelope. The key determinant of host tropism is the S1 subunit of the spike glycoprotein, composed of the receptor-binding domain (RBD) and N-terminal domain (NTD).
As a result, the humoral immune response to the spike glycoprotein represents the most robust way to tackle the infection with SARS-CoV-2. And the current vaccines indeed instigate a potent polyclonal antibody response by delivering those 'spikes' via immunization.
.jpg)
Emerging SARS-CoV-2 variants of concern
However, spike glycoprotein tends to recombine and mutate, resulting in the rise of new variants for immunogenic selection. Consequently, manifold variants of concern have augmented viral transmissibility and antibody escape, while many variants with compound spike mutations have spread since the emergence of a well-known and globally dominant D614G mutation.
More specifically, the B.1.1.7 (United Kingdom), B.1.1.248 (Brazil), B.1.351 (South Africa) and B.1.427/B.1.429 (California) lineages are especially concerning since they can partially dodge convalescent sera, monoclonal antibodies and vaccine-induced humoral immunity.
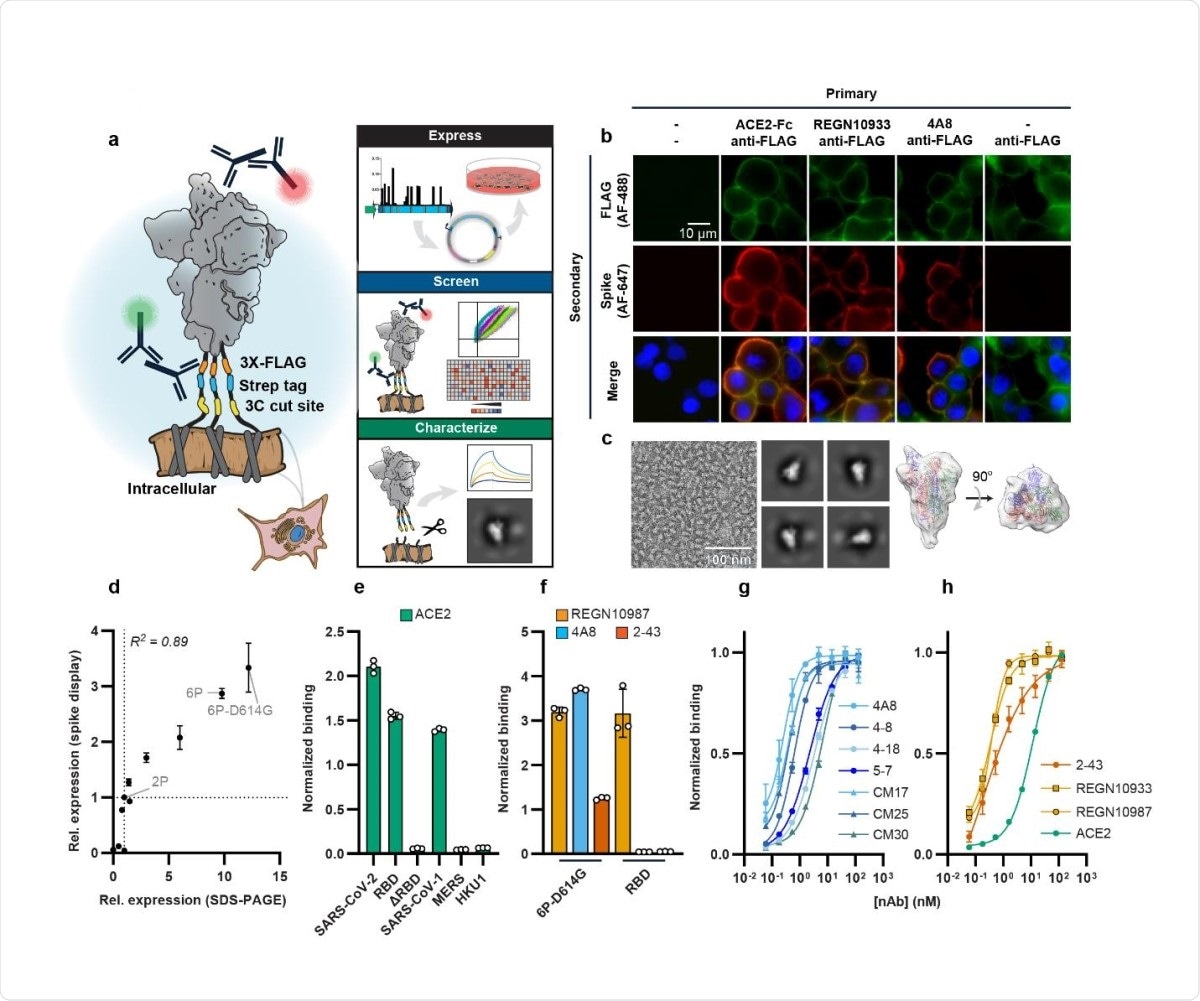
But how to characterize these spike glycoproteins from diverse coronavirus families? One rapid and high-throughput platform that has been established recently is so-called spike display, where complex spike variants are assembled via a Golden Gate cloning framework, amenable for both manual and robotically automated cloning.
In this new paper, a research group from Texas (led by Dr. Kamyab Javanmardi from the University of Texas at Austin, US) assayed approximately 200 variant SARS-CoV-2 spikes for their expression, binding to ACE2 and subsequent recognition by thirteen neutralizing antibodies.
Methodological approach
In this study, the researchers initially expressed SARS-CoV-2 spike ectodomain on the surface of human embryonic kidney (HEK293T) cells that are commonly used in experiments like these. Then they have assessed spike expression and antigenicity by utilizing flow cytometry.
In the methodologically key aspect of the study, SARS-CoV-2 spike glycoprotein variants and kindred spike homologs were swiftly constructed via Golden Gate assembly from standardized parts and acoustic liquid handling.
This study group has also measured ACE2 binding affinity of surface-displayed spikes by using non-cross reactive fluorescent secondary antibodies directed against the human (ACE2 binding) and mouse antibody Fc fragment.
Escaping neutralizing antibodies
This study highlighted a public class of epitopes in the N3 and N5 loops of SARS-CoV-2 NTD that are recognized by most of the NTD-binding neutralizing antibodies that were assayed. Albeit some clinical NTD substitutions can overturn the binding process to these epitopes, they are found at very low frequencies worldwide.
Furthermore, NTD mutations in the aforementioned viral variants of concern impact spike expression and escape a majority of NTD-targeting neutralizing antibodies. Nonetheless, two classes of NTD antibodies are still able to bind B.1.1.7 spikes and convey neutralization in pseudoviral assays.
It was also observed that Brazilian and South African variants include compensatory mutations that can increase spike expression or binding affinity. Finally, both of these variants can completely escape a potent ACE2 peptide mimic.
Unveiling antibody-spike interactions
In a nutshell, this study has shown how spike display can accelerate the characterization of important antibody-spike interactions, but also the ensuing consequences of non-synonymous spike mutations. What is also important is the fact that the whole process (i.e., from Golden Gate assembly to flow-based characterization) can be completed in less than five days.
"Downstream biophysical studies can use the cell-cleaved spikes without laborious recombinant protein purification," say study authors. "A second-generation spike display platform will increase throughput by integrating spike variants in a chromosomal locus and sorting pooled libraries for phenotypic differences," they add.
Hence, increasing throughput will enable the assessment of all circulating non-synonymous spike mutations and expeditious protein engineering necessary for pre-fusion stabilization. By complementing this approach with deep mutational scanning, we may unveil pan-coronavirus epitopes that do not change and that can be used to develop universal vaccine antigens.
*Important Notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Javanmardi, K. et al. (2021). Rapid characterization of spike variants via mammalian cell surface display. bioRxiv. https://doi.org/10.1101/2021.03.30.437622, https://www.biorxiv.org/content/10.1101/2021.03.30.437622v1
Posted in: Medical Science News | Medical Research News | Disease/Infection News | Healthcare News
Tags: ACE2, Angiotensin, Angiotensin-Converting Enzyme 2, Antibodies, Antibody, binding affinity, Cell, Cell Membrane, Cloning, Compound, Coronavirus, Coronavirus Disease COVID-19, Cytometry, Enzyme, Fc fragment, Flow Cytometry, Glycoprotein, Immune Response, Immunization, Kidney, Liquid Handling, Locus, Mutation, Polyclonal Antibody, Protein, Protein Engineering, Protein Purification, Receptor, Research, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Syndrome, Vaccine

Written by
Dr. Tomislav Meštrović
Dr. Tomislav Meštrović is a medical doctor (MD) with a Ph.D. in biomedical and health sciences, specialist in the field of clinical microbiology, and an Assistant Professor at Croatia's youngest university – University North. In addition to his interest in clinical, research and lecturing activities, his immense passion for medical writing and scientific communication goes back to his student days. He enjoys contributing back to the community. In his spare time, Tomislav is a movie buff and an avid traveler.
Source: Read Full Article
