T-cell vaccine for COVID-19 may last longer than current vaccines
The current COVID-19 vaccines are designed to trigger an antibody response to the SARS-CoV-2 spike protein, which is vulnerable to mutations that could make the vaccine less effective over time. Focusing on the T-cell instead, Penn State researchers have partnered with Evaxion Biotech on a study that is the first to demonstrate the effectiveness of an artificial intelligence-generated vaccine in a live viral challenge model. Such a vaccine may provide long-lasting immunity against future emerging variants and could be used as a model for other seasonal viral diseases like the flu.
In their study, the researchers challenged mice with a lethal dose of SARS-CoV-2 and found that 87.5% of the mice that were vaccinated with the T-cell-based vaccine survived, while only one of the control-group mice survived. Additionally, all the vaccinated mice that survived cleared the infection within 14 days post-challenge. The results were published on April 11 in Frontiers in Immunology.
“To our knowledge, this study is the first to show in vivo [in a living organism] protection against severe COVID-19 by an AI-designed T-cell vaccine,” said Girish Kirimanjeswara, associate professor of veterinary and biomedical sciences, Penn State. “Our vaccine was extremely effective at preventing severe COVID-19 in mice, and it can be easily scaled up to start testing it in humans, as well. This research also paves the way for the potential rapid design of novel T-cell vaccines against emerging and seasonal viral diseases, like influenza.”
Why do we need a T-cell-based COVID-19 vaccine when the mRNA vaccines that are already in use are so effective?
According to Kirimanjeswara, the spike protein of the SARS-CoV-2 virus is under heavy selection pressure, which can result in mutations that drive the emergence of new variants.
“This means that vaccine manufacturers will have to keep creating new vaccines that target new variants, and people have to keep getting these new vaccines,” he said.
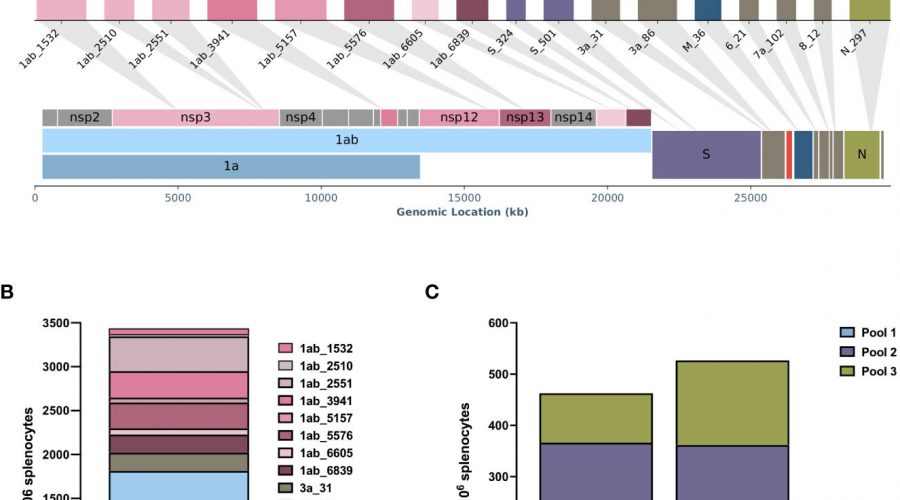
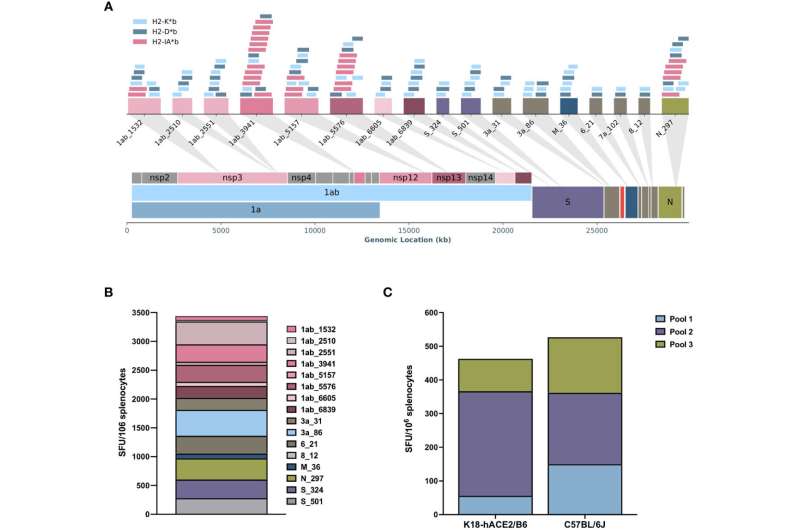
Instead of targeting the constantly mutating spike protein, the team at Evaxion Biotech designed a vaccine that included 17 epitopes from various proteins of SARS-CoV-2 that are recognized by the immune system. These epitopes elicit an immune response from a broad selection of T cells, ensuring a sustained coverage of future variants.
“The virus would have to undergo too many mutations to be able to escape this T-cell-mediated immunity, so that is one advantage,” said Kirimanjeswara. “The second advantage is that T-cell-mediated immunity is usually long-lasting, so you don’t need repeated booster doses.”

If T cells are so great at remembering foreign agents, why were the first-generation COVID-19 vaccines designed to elicit responses from antibodies?
“It’s harder and takes longer to produce a T-cell-based vaccine than an antibody-based one,” said Kirimanjeswara. “Given the urgency with which we needed a vaccine to address the COVID-19 pandemic, it makes sense that vaccine manufacturers created an antibody-based vaccine. Now that the urgency has passed, a second-generation T-cell-based vaccine could be more effective and last longer.”
According to co-author Anders Bundgaard Sørensen, project director, Evaxion Biotech, other biotechnology companies are developing T-cell-based vaccines, but this team’s vaccine uses multiple types of artificial intelligence in a platform called RAVEN (Rapidly Adaptive Viral rEspoNse) to predict ideal targets for vaccines.
“RAVEN is really adaptable,” Sørensen said. “We don’t have to wait for a new strain of a virus to arrive to develop a vaccine. Instead, we can predict what will be needed in advance. That’s not something that others are doing right now.”
Sørensen noted, “It’s much easier to get broad coverage with a T-cell vaccine, as we can include multiple epitopes targeting different proteins.”
He added that in addition to producing better COVID-19 vaccines, the RAVEN platform could be used to develop better influenza vaccines.
“Oftentimes, the influenza vaccines that are designed work only 30-40% of the time, so a lot of people end up getting sick,” he said. “As the world becomes increasingly integrated, that problem will become larger and larger. Our platform uses AI to better predict what will be needed.”
Sørensen noted that Evaxion benefited from partnering with Kirimanjeswara and his Penn State colleagues because of their deep expertise in animal models of infectious disease and because the university houses a BSL-3 laboratory in which they could safely study the SARS-CoV-2 virus.
He said, “Our results are a testament to the power of industry-university partnerships.”
More information:
Gry Persson et al, DNA immunization with in silico predicted T-cell epitopes protects against lethal SARS-CoV-2 infection in K18-hACE2 mice, Frontiers in Immunology (2023). DOI: 10.3389/fimmu.2023.1166546
Journal information:
Frontiers in Immunology
Source: Read Full Article