Study suggests women may be undertreated for obstructive sleep apnea
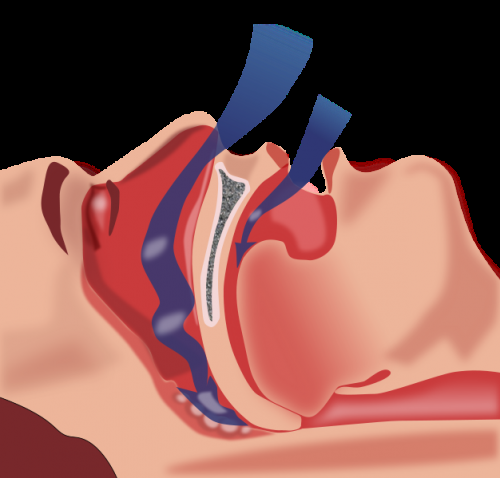
Obstructive sleep apnea (OSA) has been considered a predominantly male disease. While more women have been diagnosed with OSA in recent years, the numbers remain disproportionate, with 3-to-5 times more men than women receiving an OSA diagnosis. Investigators from Brigham and Women’s Hospital and Yale School of Medicine set out to understand this disparity and its causes. They found that a high proportion of women experienced sleep apnea during dream sleep, which is associated with adverse outcomes including cardiovascular disease. Their findings have implications for the screening, diagnosis and treatment of OSA among women and men and are published in the journal SLEEP.
“Over the years, I’ve felt strongly that sleep apnea may be an exemplar of a chronic disease that may manifest differently in men and women, from how it presents to its underlying physiology, with implications for how it should be treated,” said senior author Susan Redline, MD, MPH, a senior physician in the Division of Sleep and Circadian Disorders in the Departments of Medicine and Neurology at the Brigham. “Here, we begin to drill down to understand how sleep apnea may differ and how common scoring approaches may underestimate sleep apnea in women.”
To conduct their study, the investigators analyzed participants in the Multi-Ethnic Study of Atherosclerosis (MESA). Between 2010 and 2013, the team analyzed data from 2,057 MESA participants who underwent a comprehensive sleep study. The mean age of the study participants was 68.
Usually, home-based sleep studies only measure breathing activity, not brain activity and other criteria that can be measured in a sleep lab setting. But for this study, many parameters were measured, including brain activity and body movement.
The team compared a range of summary measures of sleep apnea severity based on the apnea-hyponea index (AHI), the number of breathing pauses per hour of sleep. An AHI greater than 15 is generally considered to indicate moderate to severe sleep apnea and is associated with increased risk of developing hypertension and mortality. The investigators calculated AHI numerous ways, some of which were more sensitive to capturing changes in breathing patterns during REM sleep (dream sleep) and non-REM sleep (other stages of sleep). The team extracted detailed measures from the overnight sleep study to also estimate some of the mechanisms that may cause sleep apnea, including measures of the collapsibility of the airway, the sensitivity of breathing patterns to changes in oxygen and changes in how quickly individuals woke up at night.
The team found that during non-REM sleep, twice as many men as women had an AHI score greater than 15. However, during REM sleep, the prevalence was the same in men and women. Among the study population, almost 60 percent of men and women met diagnostic criteria for moderately severe sleep apnea. The authors note that there is mounting evidence of an association between sleep apnea during REM sleep and adverse cardiovascular outcomes. The study also found that the physiological mechanisms that influence sleep apnea differ in men and women: women had lower loop gain (lower sensitivity to changes in ventilation), less airway collapsibility, and lower arousal threshold (more easily wake up after an apnea) in non-REM sleep. These specific aspects of sleep apnea are thought to be targets for new treatments for sleep apnea.
“We are more and more appreciating that sleep apnea is a heterogeneous disease,” said corresponding author Christine Won, MD, MSc, the director of the Women’s Sleep Health program at Yale School of Medicine. “It’s important to understand how it affects men and women differently. Understanding sex-specific mechanisms allows us to target therapy and is expected to lead to better outcomes.”
Medicare currently requires an oxygen desaturation level of 4 percent along with apnea events in order to consider someone to have OSA and receive coverage for treatment. Redline and colleagues compared this definition to other definitions in which the desaturation requirement was not as strict and took into consideration mini-awakenings—events that are not measured in most at-home sleep studies. The team found OSA rates that were almost double in women when these definitions that counted events that resulted in milder desaturation or awakenings compared to events that were only counted when larger amount of desaturation occurred.
Source: Read Full Article
