Similarities between COVID-19, cold and flu symptoms could lead to higher infections
Feeling sniffly, congested or have a sore throat and don’t know if it’s a cold, the flu or SARS-CoV-2? Researchers at York University say before heading to work or a restaurant, it’s best to test first for COVID-19 and wear a mask.
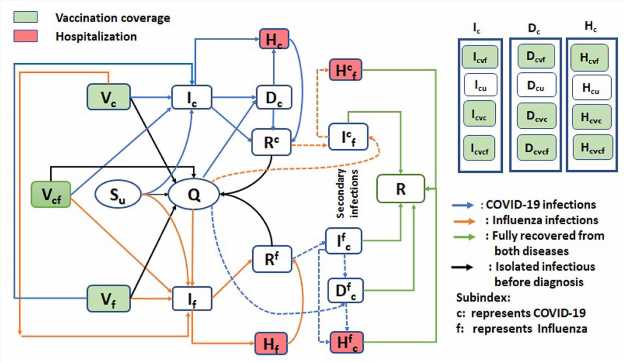
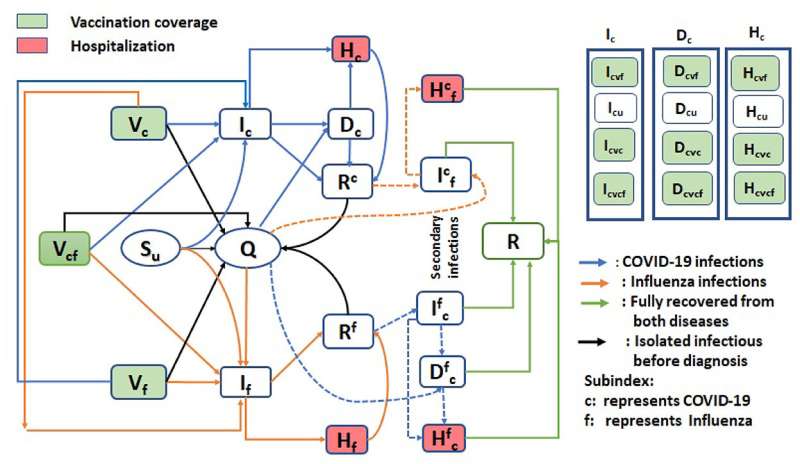
New modeling research looks at the co-circulation dynamics of influenza and COVID-19 to understand the role of vaccines, testing speed and the use of personal protection strategies, such as masking, in helping to avert COVID-19 and the flu peaking at the same time.
The researchers, including York Faculty of Science lead author and Ph.D. student Bushra Majeed, senior author Assistant Professor Woldegebriel Assefa Woldegerima, and Distinguished Research Professor and Director of the Laboratory for Industrial and Applied Mathematics Jianhong Wu, found that increasing COVID-19 daily testing capacity delays the outbreak peak time and peak size, but increases the number of flu infections.
“The reason is that people don’t need to isolate if they have the flu. By testing for COVID-19 early on, when symptoms first arise, people who test negative will continue to do their normal daily things, including heading to the office, even if they have the flu. That increases the time period when others could be infected,” says Majeed.
“Assuming you have just the flu could increase not only the rate of influenza but COVID-19. On the other hand, assuming you have COVID-19 and isolating may decrease influenza and COVID-19 infections.”
The study also found that if more people get their third or fourth booster dose of a COVID-19 vaccine, even if the influenza coverage is kept at about 35%, which is average, it will delay the peak times for both COVID-19 and the flu.
“Delaying or diminishing peak time of either the flu or COVID-19 would provide a huge benefit for our already stressed health-care system,” says Woldegerima. “Having COVID-19 and the flu co-circulating, especially as they have similar symptoms, can quickly overburden health care, as we’ve already seen, and slow testing and treatment.”
As multiple highly contagious strains of SARS-CoV-2 continue to gain traction and circulate—especially ones that are better at evading the immune system and rendering vaccines less effective—the more likely there will be new waves of COVID-19 permeating a typical flu season.
In addition, the study found that if the more people were vaccinated against both, but particularly the flu vaccine, it would reduce the peak for COVID-19 and delay the peak time for both infections, significantly.
Mask wearing, however, coupled with a moderate increase in vaccine uptake may mitigate COVID-19 and prevent an influenza outbreak. As of their last available report covering the last week of December 2022, FluWatch Canada reported there were 2,841 lab-confirmed flu cases.
The researchers say their study has important practical implications for public-health policy as it shows effectively managing and controlling influenza and COVID-19 outbreaks in the same
season relies on optimal strategies for vaccine coverage.
The paper, “Mitigating co-circulation of seasonal influenza and COVID-19 pandemic in the presence of vaccination: A mathematical modeling approach,” is published in the journal Frontiers in Public Health.
More information:
Bushra Majeed et al, Mitigating co-circulation of seasonal influenza and COVID-19 pandemic in the presence of vaccination: A mathematical modeling approach, Frontiers in Public Health (2023). DOI: 10.3389/fpubh.2022.1086849
Journal information:
Frontiers in Public Health
Source: Read Full Article