Rogue antibodies wreak havoc in severe COVID-19 cases
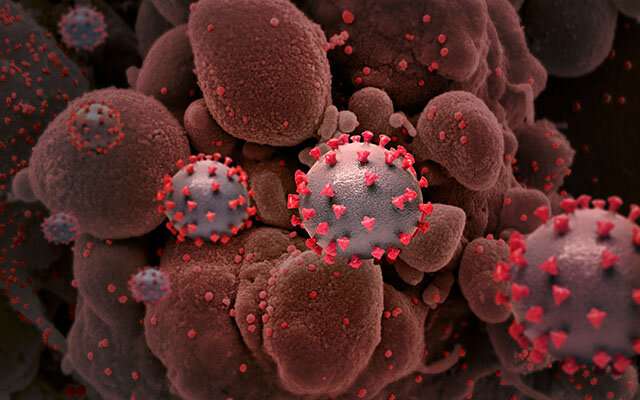
The development of antibodies to the COVID-19 virus has been the great long-term hope of ending the pandemic. However, immune system turncoats are also major culprits in severe cases of COVID-19, Yale scientists report in the journal Nature.
These autoantibodies target and react with a person’s tissues or organs similar to ones that cause autoimmune diseases such as lupus or rheumatoid arthritis. In COVID-19 cases they can attack healthy tissue in brain, blood vessels, platelets, liver, and the gastrointestinal tract, researchers report. The more autoantibodies detected, the greater the disease severity experienced by patients.
And the autoantibodies paradoxically also target and interfere with many immune system proteins that are designed to fend off infections, the study found.
“It’s a two-edge sword,” said Aaron Ring, assistant professor of immunobiology at Yale and senior author of the paper. “Antibodies are crucial to fend off infection, but some COVID-19 patients also develop antibodies that damage their own cells and tissues.”
It is clear that in many cases the presence of coronavirus drove the creation of the damaging autoantibodies, Ring said. But it is also likely that some COVID-19 patients had pre-existing autoantibodies that made them more susceptible to infection, he said. Mice with these same autoantibodies were more susceptible to infection by the COVID-19 virus and more likely to die, the authors report.
The existence of these long-lived rogue autoantibodies could also help explain why some people infected with COVID-19 can later develop lasting medical symptoms, so-called long COVID cases. “This could be the unfortunate legacy of the virus,” Ring said.
“Our findings reinforce the importance of getting vaccinated,” added co-corresponding author Akiko Iwasaki, the Waldemar Von Zedtwitz Professor of Immunobiology at Yale. “The fact that even mild infections are associated with autoantibody production underscores the potential for long-term health consequences of COVID-19.”
For the study, Ring’s lab worked with Iwasaki’s lab and members of the Yale IMPACT team—a group of scientists, scholars, and physicians developing research and clinical efforts to combat COVID-19—to screen blood samples from 194 patients who had contracted the virus, with varying degrees of severity, for the presence of autoantibodies. Specifically, they used a novel technology developed by Ring’s lab called Rapid Extracellular Antigen Profiling (REAP) to identify autoantibody interactions with nearly 3,000 human proteins.
Source: Read Full Article
