Real-time pneumonia test for COVID-19 patients aiding faster therapy
An ongoing study involving UEA, which quickly identifies the cause of a patient’s pneumonia enabling earlier optimization of treatment, is being re-purposed to assist with the coronavirus pandemic.
Pneumonia is one of the main symptoms of severe COVID-19 disease and, because many critically ill COVID-19 patients can no longer breathe by themselves they are put onto mechanical ventilators.
These pump air through a tube into the lungs, helping the patient to survive. However, unfortunately the ventilation also increases the risk of bacteria entering the lungs, establishing a further infection known as “secondary pneumonia.”
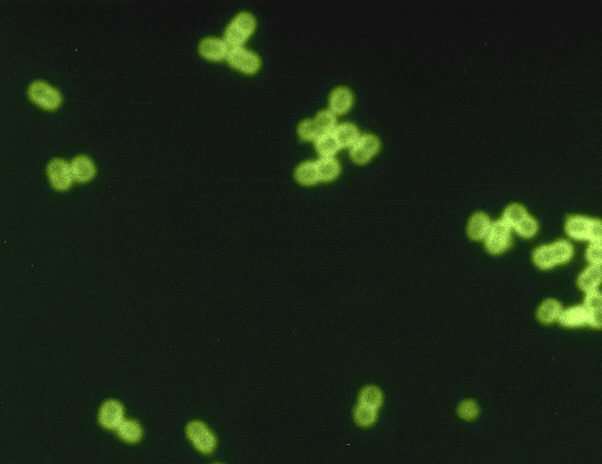
The INHALE trial, led by UCL in collaboration with UEA and the Norwich Clinical Trials Unit, is evaluating cutting-edge ‘molecular diagnostics’ to identify bacteria directly from pneumonia patients’ sputum (fluid produced in lungs), without the need for lab culture.
The test, developed by biotech company bioMerieux BioFire, can pinpoint 26 pneumonia pathogens and can detect whether these have critical antibiotic resistances.
A test result is obtained in around one hour and the information aims to give clinicians early guidance on which antibiotics to use—meaning ones likely to be active against the bacteria detected.
It also discourages the use of unnecessary antibiotics, which can contribute to the development of further antibiotic resistance.
INHALE has been evaluating this approach in ‘run of the mill’ ventilator pneumonia patients at 12 ICUs in England for the past six months.
Now, in the present pandemic, the study is being temporarily refocused to investigate the secondary bacterial pneumonias that COVID-19 patients get, and to guide their treatment.
It has already been used in over 50 patients at hospitals including UCLH, the Royal Free, Watford General, Chelsea and Westminster and Liverpool University Hospitals.
The study’s Co-Chief Investigator, Prof David Livermore from UEA’s Norwich Medical School, said: “We know that some COVID patients get secondary pneumonias but it’s a new disease and no one knows what types of bacteria are most likely. This refocusing of INHALE aims to provide that information, and to do it quickly enough to support the treatment of individual patients.”
INHALE Study Investigator, Dr. Vicky Enne from UCL said: “Bacterial pneumonias need urgent antibiotic treatment and left untreated can cause death: administering the right antibiotics as quickly as possible at diagnosis is therefore critical to survival.
“Unfortunately it takes two to three days to grow the bacteria in the laboratory, so it’s conventional to start with broad-spectrum antibiotics, active against many types of bacteria, then to refine treatment once the lab results come through.
“To significantly reduce this delay our study aims to accurately identify the bacteria in under an hour, thereby allowing doctors to pinpoint the best antibiotic in quick time.
“Antibiotic resistance is as much of a threat during the pandemic as it was before COVID-19. The BioFire test allows doctors to give the right antibiotics to those that need them and prevents their unnecessary use, thus ensuring we are doing everything we can to spare these valuable drugs.”
Dr. David Brealey, ICU Consultant at UCLH and Senior Lecturer at UCL Medicine, said: “Having the BioFire to help identify pneumonia has been invaluable in managing COVID-19 patients on the ICU at UCLH. These patients are so sick, we cannot wait days to get a result back from the lab, and this machine gives the result direct to the treating clinician within the hour. Real, actionable intelligence is making a difference to the way we treat our patients.”
Study Chief Investigator, Dr. Vanya Gant, Consultant Microbiologist at UCLH and Honorary Senior Lecturer at UCL Infection & Immunity, said: “The INHALE team are very proud to have been able to so rapidly adapt the paused INHALE clinical trial to deliver vital clinical results to front line ICU clinicians in an hour by repurposing our testing equipment and infrastructures. And what’s more—we’ve put in analyses that will tell us what this might mean in terms of patient benefit.”
Source: Read Full Article
