Cancer study highlights racial disparities for patients facing dual diagnoses
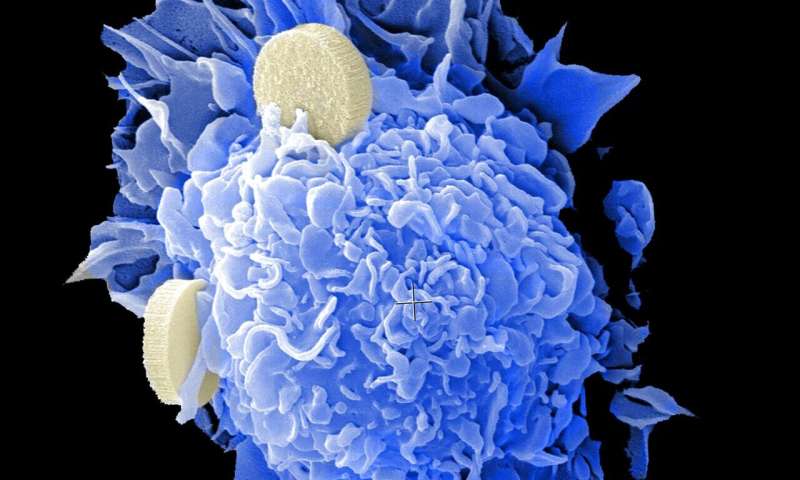
The COVID-19 and Cancer Consortium (CCC19) published new findings in the Annals of Oncology, showing heightened mortality and racial disparities for patients with cancer diagnosed with SARS-CoV-2 infection.
After reviewing detailed information from almost 5,000 patients with active or past cancer and laboratory-confirmed COVID-19 diagnosis, CCC19 study authors found associations among laboratory measures, clinical factors—including older age, hematological malignancy and recent chemotherapy—and poor clinical outcomes. Of the patients in the study with COVID-19 and cancer, 58% required hospitalization and 14% died within 30 days—compared with a COVID-19 death rate below 2% for the general population. The 30-day death rate decreased over time, a finding that needs investigation.
“This study provides an in depth take on several timely and really pressing issues in healthcare—highlighting the effect of COVID-19 on mortality, need for hospitalization, ICU care and mechanical ventilation, while it also illustrated racial disparities in cancer care,” said co-first author Petros Grivas, MD, Ph.D., a medical oncologist at Seattle Cancer Care Alliance, associate professor at University of Washington and associate member at Fred Hutchinson Cancer Research Center. “Our findings also indicated a potential association between specific anti-cancer therapies and 30-day mortality, suggesting a need for caution and careful risk-benefit assessment in utilizing therapies.”
Other key findings include higher COVID-19 severity in older patients, men, obese individuals, those with medical comorbidities, as well as Hispanic and Black populations. Due to the increased sample size, the study was able to quantify the pandemic’s disproportionate impact on Black, Indigenous and other People of Color (BIPOC) patients with cancer.
“One of the most notable findings was that BIPOC patients with cancer had worse COVID-19 outcomes than White patients—something we hadn’t appreciated earlier due to smaller total case numbers,” said Jeremy L. Warner MD, Associate Professor of Medicine (Hematology/Oncology) and Biomedical Informatics at Vanderbilt University. “While the reasons are multiple, we suspect this is an extension of the healthcare disparities that have affected the general population throughout the pandemic, including unequal healthcare access and systemic racism.”
The study also revealed numerous contributing laboratory parameters to more severe COVID-19 illness in patients with active or past cancer, including low or high ALC, high ANC, low platelets, abnormal creatinine, troponin, LDH or CRP.
Source: Read Full Article
