Intranasal vaccination produces potent systemic immunity against HIV and SARS-CoV-2 in animal models
Even though most viruses cause infection directly through mucosal cells, the vast majority of vaccines are administered intramuscularly in a cellular mismatch that doesn’t always produce optimum immunity.
SARS-CoV-2 infects through the nasal mucosa, HIV via the genital and anal mucosa. But those two aren’t alone, a host of other viruses, including those that cause influenza, measles and polio—along with many, many others—infect humans through mucosal tissue.
Now, a large multi-institution team of scientists is working on an intranasal method of immunization to determine if it’s possible to produce effective protection against HIV and SARS-CoV-2 via vaccination directly into mucosal cells. Scientists accomplished these feats by developing a method to deliver vaccine proteins across a sometimes unyielding mucosal border. To date, the research has been conducted in in animal models—mice and nonhuman primates—but results so far suggest a promising method to test in human clinical trials.
“To combat the HIV epidemic and emerging threats such as SARS-CoV-2, immunization strategies are needed that elicit protection at mucosal portals of pathogen entry,” wrote Brittany Hartwell of the Massachusetts Institute of Technology and colleagues from multiple collaborating U.S. institutions. Their investigation is published in Science Translational Medicine.
“Immunization directly through airway surfaces is effective in driving mucosal immunity, but poor vaccine uptake across the mucus and epithelial lining is a limitation. The major blood protein albumin is constitutively transcytosed bidirectionally across the airway epithelium.”
Albumin has often been inhospitable to vaccine payloads making their way into mucosal cells. As a result of that stumbling block, uptake of vaccine via mucosal routes has been limited. By developing a completely new strategy to get the payload effectively into mucosal cells, the group of scientific collaborators is on the verge of ushering in a new-to-science innovation that ensures the delivery of immunizing proteins.
In their journal report, Hartwell and colleagues present what they call an amph-protein strategy, which allows immune-stimulating proteins to “hitchhike” across mucosal surfaces. Their amph-proteins consist of viral proteins conjugated to an amphiphilic tail that binds albumin, a blood protein, and thus enables crossing the mucosa by interacting with the neonatal Fc receptor. The neonatal Fc receptor, or FcRn, is also known as the Brambell receptor. It protects the antibody, IgG, or immunoglobulin-G and albumin from catabolism and also ushers IgG across epithelial cells.
The team turned to animal models to determine whether this experimental intranasal method could effectively deliver immunizing proteins through mucosal surfaces and produce potent vaccine immunity against two notorious viruses: HIV and SARS-CoV-2. The study demonstrated that intranasal vaccination produced systemic immunity.
Going into the experiments scientists knew that intranasal vaccines can elicit stronger and more protective antibody responses than injected intramuscular vaccines. But they were also well aware that some experimental mucosal vaccines have been limited by poor vaccine uptake across mucosal linings.
What they wanted to find out is whether it was possible to tweak how the vaccine is delivered and, in turn, demonstrate how the mucosal vaccination route leads to a substantially more powerful antibody response. If they could do that—and their research ultimately proved that they could—then they would be on the cusp of a vaccine that could provide protection against HIV and SARS-CoV-2—and any potential variant. Their first step was developing a vaccine platform that could be tested in mice and nonhuman primates.
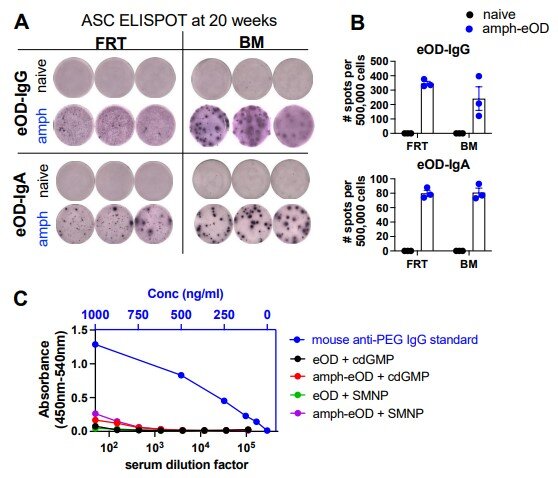
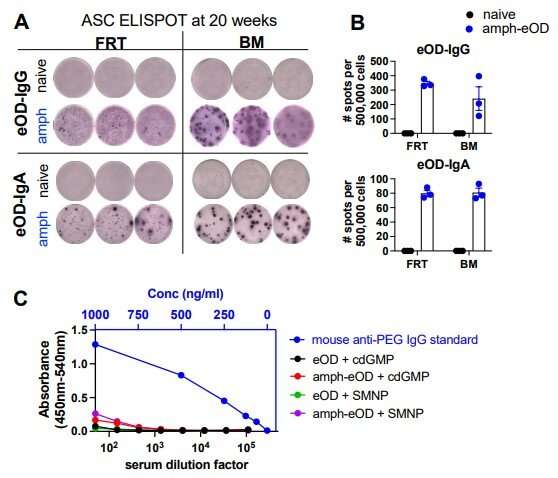
When formulated with the HIV protein Env gp120, or the receptor binding domain of SARS-CoV-2, the amph-proteins evoked strong antiviral antibody responses in serum and nasal mucosa in immunized mice and nonhuman primates.
“Intranasal immunization with amph-conjugated HIV Env gp120 or SARS-CoV-2 receptor binding domain proteins elicited 100- to 1000-fold higher antigen-specific IgG and IgA titers in the serum, upper and lower respiratory mucosa, and distal genitourinary mucosae of mice compared to unmodified protein,” Hartwell wrote, referring to the antibodies immunoglobulin-G and immunoglobulin-A.
“Amph receptor binding domain immunization induced high titers of SARS-CoV-2–neutralizing antibodies in serum, nasal washes, and bronchoalveolar lavage. Furthermore, intranasal amph-protein immunization in rhesus macaques elicited 10-fold higher antigen-specific IgG and IgA responses in the serum and nasal mucosa compared to unmodified protein, supporting the translational potential of this approach,” Hartwell asserted in the paper.
The results suggest that using amph-protein vaccines to deliver antigen across mucosal epithelia is a promising strategy to promote mucosal immunity against HIV, SARS-CoV-2, and eventually other infectious diseases as additional vaccines using this strategy are developed. “Amph-proteins persisted in the nasal mucosa of mice and nonhuman primates and exhibited increased uptake into the tissue … leading to enhanced germinal center responses in nasal-associated lymphoid tissue,” Hartwell concluded.
Source: Read Full Article