How COVID Affects Your Heart, According to a Cardiologist
As the COVID-19 pandemic continues to infect millions of people around the world, researchers are learning more about how the virus affects various organs in the body. While it was initially thought to be a respiratory illness, it's now clear that it attacks far more than just the lungs. Doctors are especially concerned about how it may impact the heart. Dr. Jennifer Haythe, critical care cardiologist at Columbia University Center and member of the PEOPLE Health Squad, shares what experts know about how COVID-19 impacts the cardiovascular system.

How does COVID-19 impact the heart?
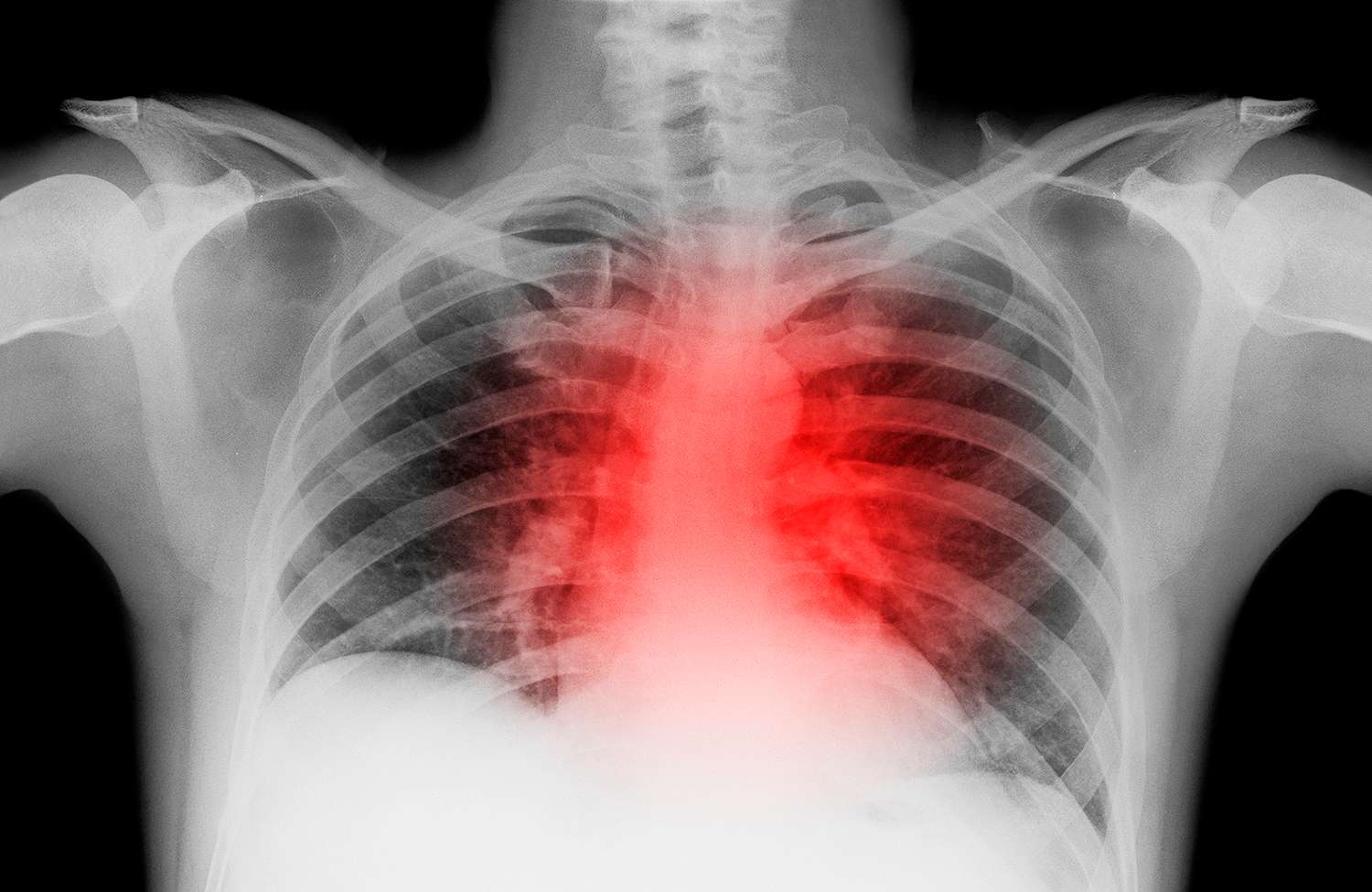
One way COVID affects the heart is that it can cause myocarditis, or an inflammation of the heart muscle, which can cause different kinds of symptoms, including chest pain, abnormal heart rhythms, and even reduced heart function.
Another way that we're seeing COVID affect the heart is by causing significant arrhythmias. People come in with heart rhythms that cause their blood pressure to drop, or cause them to feel palpitations, or even cause them to require CPR.
The third is heart failure syndrome. COVID can affect the heart cells themselves, and cause heart function to become reduced, so people have symptoms like shortness of breath, fluid in the lungs and swelling of the feet.
What is the biggest concern for people with known heart issues if they're diagnosed with COVID?
People with underlying heart disease or impaired vasculature — meaning they have pre-existing diabetes or high blood pressure or obesity — those people are at increased risk. They should look out for chest pain, shortness of breath, feeling lightheaded, feeling like they're near fainting, or actually fainting. Those are things that should warrant going to the emergency room, or certainly calling your doctor.
COVID has emerged as a virus that really affects the blood vessels in the body — and obviously, the heart is sort of the biggest blood vessel of all. We know that it affects the blood vessels in the brain and causes strokes and causes clots to form in the blood vessels of the lungs. It causes rashes to form in people's hands due to the clotting of the small blood vessels in the skin. It causes kidney failure from the same mechanism affecting the vasculature of the kidneys. And the heart is the same.
What is the biggest misconception that people have about COVID and heart health?
People think that if they have any kind of heart disease, that they're going to die of COVID. And I want to reassure people that that's not the case. So if you've had heart surgery, or a valve replacement, that doesn't necessarily mean that you're going to die of COVID. What it does mean, though, is that you may have some risk factors that could lead to more severe COVID. We think that it's probably because COVID causes this abnormal inflammation of the blood vessels. And so you should take a COVID infection more seriously, but not panic.
What has your COVID experience been like on the front lines?
I work in the ICU at Columbia — which is part of New York-Presbyterian Hospital — and basically all of our hospital was overwhelmingly COVID patients. In the intensive care unit, we were doubling up our rooms. Normally an ICU room is one patient to a room, so we had to put two patients to a room, and all of the operating rooms were filled with COVID patients. It was definitely very overwhelming and felt very disturbing for everybody, and scary and stressful, and a lot of patients died. It came all at once very suddenly. Now the COVID experience is different. We know a bit better how to treat it. People have better PPE, and some people are vaccinated.

How is it different to treat COVID patients now versus when it first hit the United States last year?
The hospital feels like it's still functioning as a hospital, whereas before it was shut down and only taking care of COVID. Now we're still seeing our heart patients, and we're still doing elective procedures, and we're still doing surgery. And the fear factor is gone a little bit.
But I think that there's a weariness to how people are feeling. There's still a lot of young, middle-aged people on breathing tubes, dying in the intensive care unit. And that's stressful for everybody and takes its toll.
What else should readers know about heart health for American Heart Month?
For women, heart disease is the number one cause of death in this country. But 85% of heart disease can probably be prevented with good early management. When you are between 18 and 40, if you actually eat a healthy diet, stay away from toxins, exercise and stay fit, you can reduce heart disease in your 40s, 50s, 60s, 70s and 80s. Even if you're 40 to 60 now, you can still do a lot of things to reverse your risk and reduce your chances of heart disease, like seeing your doctor every year and getting screened for risk factors.
Source: Read Full Article
