Half-dose TNK for STEMI Without Timely PCI: STREAM-2
Giving half-dose thrombolytic to ST-elevation myocardial infarction (STEMI) patients who are going to have a delay in receiving primary percutaneous coronary intervention (PCI), provided effective reperfusion based on ST-deviation resolution and angiographic results in the STREAM-2 trial.
“Especially in community hospitals and in worldwide situations where primary PCI is difficult to access, this is a very legitimate and effective strategy,” study chair Paul Armstrong, MD, University of Alberta, Edmonton, Canada, concluded.
Armstrong presented the STREAM-2 trial at the recent American College of Cardiology (ACC) Scientific Session/World Congress of Cardiology (WCC) 2023.
During the presentation, Armstrong explained that a significant percentage of STEMI patients transferred from community hospitals do not get primary PCI within the recommended 2 hours after first medical contact, resulting in increased mortality.
Previous trials (ASSENT and STREAM-1) have shown increasing rates of intracranial hemorrhage (ICH) and major non-intracranial bleeding in the older population with full-dose thrombolysis, with rates starting to increase from age 60, he noted.
The current STREAM-2 study was therefore conducted to evaluate the efficacy and safety of half-dose tenecteplase (TNK) as part of a pharmaco-invasive strategy in older STEMI patients as compared with primary PCI.
The international trial enrolled 609 patients aged 60 years or older and presenting within 3 hours of symptom onset of STEMI but unable to undergo primary PCI within 1 hour. They were randomly assigned to half-dose tenecteplase, given either in the ambulance or at the community hospital, or to primary PCI (controls). The mean age was 70 years in the tenecteplase group and 71 in the control group.
All patients received aspirin 150 to 325 mg. The lytic group received clopidogrel at an initial dose of 300 mg then 75 mg daily, and enoxaparin (30 mg IV bolus then 1 mg/kg subcutaneously every 12 hours in those younger than 75, and no IV bolus then 0.75 mg/kg every 12 hours in those older than 75.)
The control group received antiplatelet and anticoagulant therapy according to local practice.
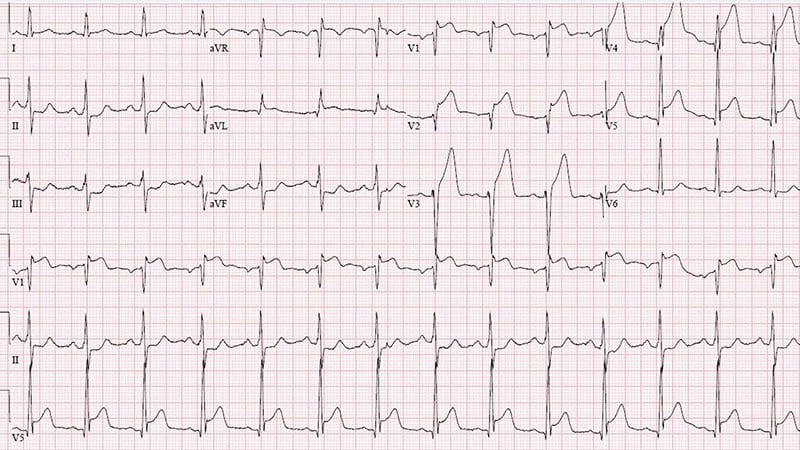
The lytic group underwent an ECG 90 minutes after the bolus tenecteplase, or earlier if clinically indicated. If this showed less than 50% resolution of ST elevation, patients received immediate angiography and rescue PCI. If the ECG showed more than 50% resolution of ST elevation, patients underwent angiography later (6 to 24 hours) and PCI if required.
The efficacy endpoints of primary interest were the percentage of patients with more than 50% ST-segment resolution after tenecteplase and before and after PCI, the need for rescue PCI, and the combined clinical endpoint of death, cardiogenic shock, reinfarction, and heart failure at 30 days. Key safety outcomes were ICH and major non-ICH bleeding within 30 days.
Results showed that in the tenecteplase group, thrombolysis was given at an average of 110 minutes after symptom onset. The control group underwent primary PCI at an average of 190 minutes after symptom onset.
“There is an 80-minute difference between the time of thrombolysis in the lytic group and the time of primary PCI in the control group. That’s the window of opportunity, meaning that these patients in the lytic group are getting some reperfusion earlier,” Armstrong told theheart.org | Medscape Cardiology.
Results showed that patients who received lytic therapy had better resolution of the ST elevation. The worst lead ST resolution of more than 50% occurred in 85.2% of the lytic patents vs 78.4% of the control group (P = .05).
The sum of the residual ST deviation was also lower in the lytic group (4.5 mm vs 5.5 mms; P = .02), showing better resolution of ischemia.
Angiographic results before PCI showed TIMI-3 flow in 53.8% of the lytic groups vs 18.9% of the control group (P < .001).
Rescue PCI was performed in 34% of the lytic group and 86% of the lytic group received PCI within 24 hours. After PCI, TIMI-3 flow occurred in 87% of both groups.
The study was underpowered to show an effect on clinical events, Armstrong noted, but the composite endpoint of death/heart failure, shock, recurrent MI at 30 days occurred in 12.8% of the lytic group and 13.3% of the control group, a nonsignificant difference.
Subgroup analysis suggested that among those randomized within 1 hour of symptom onset, there was a significant benefit in clinical outcomes in the lytic group, but Armstrong cautioned that this result was based on small numbers.
In terms of safety, ICH occurred in six patients in the lytic group (1.5%) vs zero patients in the control group.
“The ICH rate is the same as we saw in the STREAM-1 trial with full dose tenecteplase,” Armstrong said. “And we had obviously hoped that the ICH rate would have been less with the half dose in STREAM-2.”
But he pointed out that none of the patients who had ICH were older than age 75 years, which he said was reassuring, and 3 of the 6 patients with ICH had significant protocol violations.
“Two patients at the same site got excessive anticoagulation with IV heparin during a rescue procedure where there was poor communication between the ambulance system and the cath lab. And the third patient (a 74-year-old female) should not have been randomized because her blood pressure was too high,” he noted.
“There is always a risk of ICH with thrombolysis, but we believe that if everyone had paid attention to guidelines and contraindications, the ICH rate would have been acceptable,” he added.
Armstrong also pointed out that the overall event rates in both groups were “strikingly lower than expected,” and there was also a “remarkably low” systemic bleeding rate in the lytic group (1.3%), which he attributed to the high use of radial catheterization preventing systemic bleeding, which he said has historically plagued the whole lytic field.
“Reasonable Strategy”
Commenting on the study for theheart.org | Medscape Cardiology, Deepak Bhatt, MD, Mount Sinai Health System, New York City, said: “This is an interesting, modest-sized trial of older patients with STEMI when there was going to be an anticipated delay in the ability to perform timely PCI. Overall, the ischemic event rates were similar in the two arms. Thus, while the pharmaco-invasive strategy could be utilized, there did not seem to be a compelling reason to do so. However, potentially in parts of the world where even longer delays to PCI might occur, this seems like a reasonable strategy to consider.”
He noted that, even with the reduced dose lytic, there were more intracranial hemorrhages in the pharmaco-invasive arm, “so that if this approach is being used, concomitant anticoagulation and blood pressure need to be assessed very carefully.”
“Making sure that timely PCI can be accessed in rural areas, congested cities, and lower-income countries seems like a good investment of healthcare dollars — and this is already happening in many regions of the world,” Bhatt concluded.
STREAM-2 was an investigators-initiated study sponsored by University of Leuven and financially co-supported by Boehringer Ingelheim.
American College of Cardiology (ACC) Scientific Session/World Congress of Cardiology (WCC) 2023: Late-Breaking Clinical Trials. Presented March 5, 2023.
For more from theheart.org | Medscape Cardiology, follow us on Twitter and Facebook
Source: Read Full Article