Detecting depression and partner violence risk during pregnancy
Carnegie Mellon University engineering and public policy researchers Kristen Allen, a Ph.D. student, and Alex Davis, an associate professor, have new research that could complement the ability of doctors to aid recently or currently pregnant individuals who experience depression or intimate partner violence.
The new research, done in collaboration with Tamar Krishnamurti, assistant professor at the University of Pittsburgh School of Medicine, uses natural language processing on text entries completed by pre- and postpartum participants to predict the likelihood that they may be experiencing depression or intimate partner violence, as indicated through validated measures. Their results also pointed toward commonly repeated themes and topics that can broaden our understanding of potential risks.
Depression and intimate partner violence are serious concerns that can be difficult to identify within the limited confines of standard medical practice. A partner experiencing violence at home may fear reprisal from their abuser for speaking up, while social pressure and expectations about pregnancy may prevent pregnant individuals from disclosing or even recognizing their depression. Medical staff may find it difficult to spot the signs of either in routine pre- and postnatal care if problems occur between visits, or if individuals are unable to disclose them during visits. “The early postpartum period is a particular time of concern,” says Krishnamurti, “because birth-giving people have suddenly transitioned from seeing their prenatal care provider regularly to focusing on their new infant and that infant’s pediatric care needs.”
In Allen, Davis and Krishnamurti’s study, participants completed three responses: the first was a series of open-ended questions, the second was closed-form multiple choice, and the third was several risk assessments adapted from existing depression and intimate partner violence batteries. Open-ended questions asked participants to discuss their mood, recent experiences and feelings about pregnancy or motherhood.
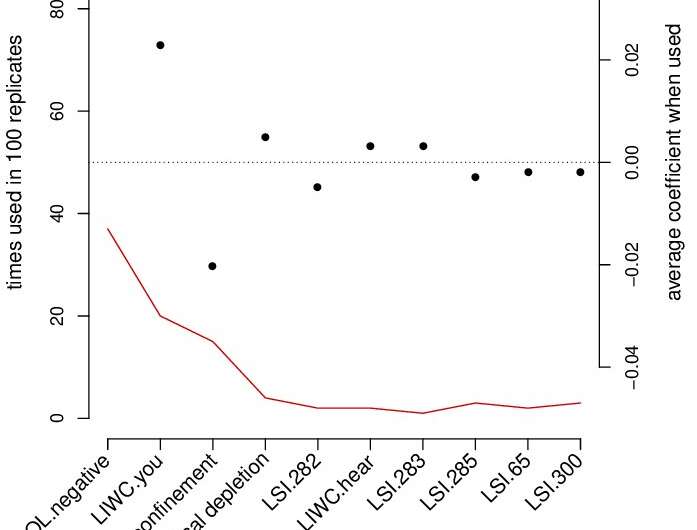
Using responses from more than 300 perinatal participants, the team conducted their analyses by applying machine learning methods for language processing to extract information from journal entries on a word-by-word basis to identify their connotation, denotation and focus. They also used topic modeling and indexing methods to weight words by topic, allowing them to quantify the likely subject of a statement.
The features they identified were informative indicators for the presence or absence of depression, while closed-form questions about partner conflict were better at predicting intimate partner violence. The group plans to expand this study to a longitudinal design with more participants over a span of years. Assessments like this, implemented between pre- and postnatal care, could be adopted to help providers prepare to learn more during in-person interaction.
For example, Davis and Krishnamurti are using a mobile health application called MyHealthyPregnancy in their ongoing research to explore these questions with those who may feel uncomfortable or unable to disclose information in a standard medical environment.
“The results suggest that open-ended text can be used to provide additional signals to health-care providers about depression, along with some of the reasons pregnant individuals might be depressed,” concluded Davis. “This can help address gaps in care between prenatal visits, as well as address biases during visits, where there may not be enough time for discussion, or where reliance on fallible memory leads to misattribution. Of course, any implementation in the real-world requires carefully communicating the purpose of the journal entries to pregnant individuals to obtain their informed consent.”
The goal is to broaden understanding of how risks manifest in language, to provide as many opportunities as possible for medical practitioners to spot signs of depression and intimate partner violence, and to offer them additional tools to support patients. For those practitioners, this study also has identified particular feelings expressed by participants that might be indicators of risks.
One cue for potential intimate partner violence were feelings of a “lack of support,” while clues for depression included a high negative or low positive sentiment, and a “physical depletion” topic indicating exhaustion. Information like this is not only useful for diagnosing the problem, but also can offer doctors and practitioners additional insights into how violence is perpetrated and conditions like depression manifest.
Source: Read Full Article
