‘Amaurosis Fugax’ may affect the eyes in week leading up to a stroke
Chris Fountain says he ‘felt really stupid’ after mini-stroke
We use your sign-up to provide content in ways you’ve consented to and to improve our understanding of you. This may include adverts from us and 3rd parties based on our understanding. You can unsubscribe at any time. More info
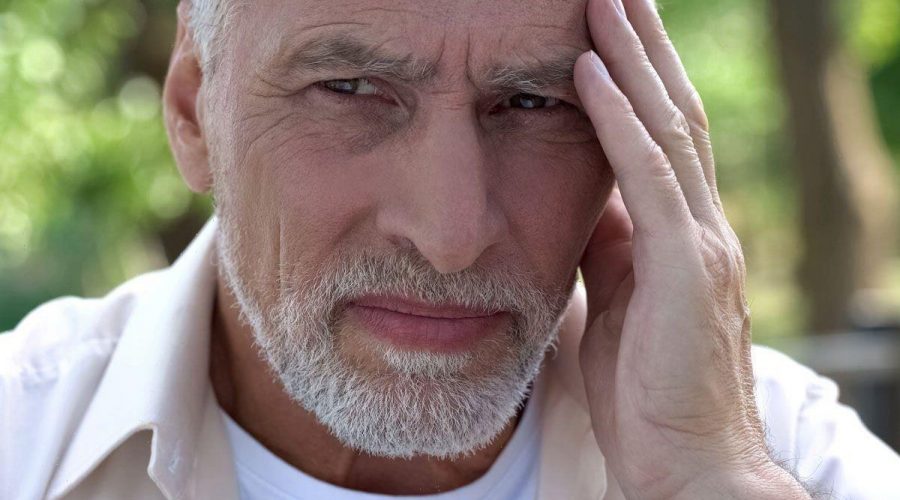
A stroke can be defined as an injury in the brain that results from an obstruction in the blood flow. As the organ becomes deprived of vital oxygen, the body’s systems start to shut down. Unfortunately, strokes typically strike with no forewarning, which is what renders the disease so deadly. Sometimes, however, changes in vision can occur in the days or weeks leading up to a stroke.
Studies have shown that up to 43 percent of stroke patients experience mini-stroke symptoms up to a week before having a full-blown ischaemic attack (TIA).
This makes TIAs a major precursor to having a major stroke and suggests that patients who experience symptoms should be seen by a doctor for examination immediately.
The symptoms in TIA rarely last longer than 24 hours, but some reports describe long-lasting symptoms.
“Since the immediate signs and symptoms of TIA are identical, it’s important to seek medical attention,” says the Mayo Clinic.

The main difference in the symptoms is the severity of their manifestation, as a stroke will be triggered by a more severe variant of blood flow dysfunction.
Gary Bartlett, from the Beversbrook Medical Centre, explained: “Some people that suffer a stroke might notice a sudden loss of vision in one eye, sometimes with no pain.
“Sometimes, people might notice a dark area or shadow in their vision that affects the upper or lower half of their visual field.
“Amaurosis Fugax is the transient loss of vision in one eye usually due to a transient ischaemic attack (TIA) commonly known as a mini-stroke.
“Patients often describe a curtain coming down vertically into the field of vision in one eye.”
The prognosis for a stroke patient is significantly worse, so addressing TIA signs when they emerge could have life-saving implications.
In fact, the Mayo Clinic explains that “about one in three people who have a TIA will eventually have a stroke, with about half occurring within a year after the TIA”.
Although a TIA typically occurs without warning, some people may feel temporary numbness, weakness or tingling in one arm or leg, known as para-esthesia.

Para-esthesia describes abnormal sensations, including feelings of pins and needles, tingling, and pricking.
Alternatively, it’s been described as the feeling of ants crawling over/under the skin.
Symptoms like tingling suggest a build-up of plaque in the arteries has compromised the sensory nervous system.
Alternatively, a TIA patient may experience problems with speech or balance.

This occurs because a blood clot has formed inside the artery, which is also due to a build-up of plaque.
Lowering blood pressure and cholesterol substantially reduces the risk of having a stroke.
The NHS states: “The best to help prevent a stroke is to eat a healthy diet, exercise regularly and avoid smoking and drinking too much.”
These lifestyle measures can help reduce the risk of other stroke precursors like arterial clogging and atrial fibrillation.
Source: Read Full Article